Primary Health Care Authority
Table of contents
- Appendix A: Terms and Conditions for Primary Health Care Authority
- 1. Summary
- 2. Objectives and Results
- 3. Legal and Policy Authority
- 4. Eligible Recipients and Annual Maximum Amount Payable
- 5. Eligible Expenditures
- 6. Stacking Provisions
- 7. Basis and Timing of Payment
- 8. Application Requirements
- 9. Due Diligence in Managing and Administering the Transfer Payment Guidelines
- 10. Audit Framework
- 11. Official Languages
- 12. Other Terms and Conditions
- 13. Non-Monetary Contributions
- 14. Funding Approaches
- Appendix H-1: Funding approaches
- Appendix H-2: Eligible activities
- Appendix H-3: Summary of requirements for due diligence
Appendix A: Terms and Conditions for Primary Health Care Authority
Effective date: December 1, 2021
1. Summary
1.1 FNIHB General Context
The First Nations and Inuit Health Branch (FNIHB) aims to provide effective, sustainable, and culturally appropriate health programs and services that contribute to the reduction of gaps in health status between First Nations and Inuit and other Canadians.
FNIHB's objectives are to support the health needs of First Nations and Inuit by: ensuring availability of, and access to, quality health services; supporting greater control of the health system by First Nations and Inuit; and, supporting the improvement of First Nations health programs and services through improved integration, harmonization, and alignment with provincial/territorial health systems.
In pursuing these objectives, FNIHB funds or provides a range of health programs and services to First Nations and InuitFootnote 1, including:
- clinical and client care services in approximately 138 remote-isolated and isolated First Nation communities;
- home and community care in 657 First Nation and Inuit communities;
- community-based health programs, focussing on healthy child development, mental wellness and healthy living, provided to approximately 600 First Nations and 50 Inuit communities;
- public health programs to all First Nation communities, including communicable disease control, and environmental public health monitoring and inspections; and,
- Non-Insured Health Benefits to status Indians and recognized Inuit, regardless of residence, in Canada.
Improving the health of Indigenous Peoples is a shared responsibility between federal, provincial/territorial and Indigenous partners. To improve health systems to better meet the needs of First Nations and Inuit, FNIHB works with its partners to develop sustainable, long-term, integrated solutions, through dedicated and collaborative efforts, including developing partnerships between provincial governments and First Nations to integrate federal and provincial health systems. FNIHB also supports the improved capacity of First Nations and Inuit communities to address their own unique health needs by increasing their control over health program design and delivery.
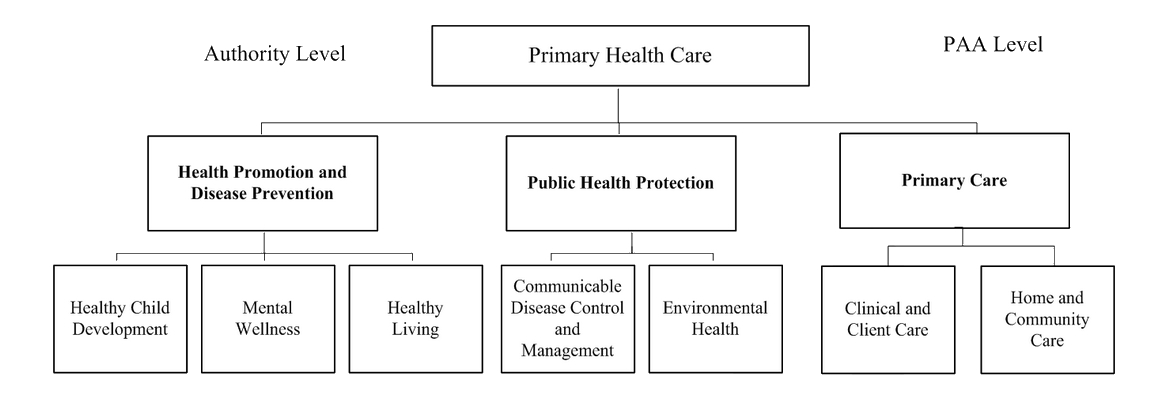
Long text description for Primary Health Care figure
The Authority/PAA level "Primary Health Care" is divided in three categories; Health Promotion and Disease Prevention, Public Health Protection and Primary Care. The first category, Health Promotion, is comprised of three sub-categories; Healthy Child Development, Mental Wellness and Healthy Living. The second category, Public Health Protection, is comprised of two sub-categories; Communicable Disease Control and Management and Environmental Health. The third category, Primary Care is comprised of two sub-categories; Clinical and Client Care and Home and Community Care.
2. Objectives and Results
2.1 Primary Health Care Authority
The Primary Health Care Activity funds a suite of programs, services and strategies provided primarily to First Nations and Inuit individuals, families and communities living on-reserve or in Inuit communities. It encompasses health promotion and disease prevention programs to improve health outcomes and reduce health risks, public health protection, including surveillance, to prevent and/or mitigate human health risks associated with communicable diseases and exposure to environmental hazards, and primary care where individuals are provided diagnostic, curative, rehabilitative, supportive, palliative/end-of-life care and referral services. All of these services will be provided by qualified health providers who have the necessary competencies and meet the regulatory and legislative requirements of the provinces and territories in which they practice.
Mandatory Programs/Services
Mandatory programs are those that have a direct impact on the health and safety of community members and the population. They have a strong public health and/or clinical component and require that health staff have certain credentials/certification/licensing and meet practice standards to ensure quality public health and client care services are provided.
Mandatory Programs within the Primary Health Care Activity include:
- Communicable Disease Control and Management sub-sub activity
- Clinical and Client Care sub-sub activity
- Home and Community Care sub-sub activity
- Environmental Public Health within the Environmental Health sub-sub activity
2.1.1 Health Promotion and Disease Prevention Sub-Activity
The Health Promotion and Disease Prevention sub-activity funds and supports a suite of community-based programs, services, initiatives and strategies that collectively aim to reduce the disparities and improve the health outcomes of First Nations and Inuit individuals, families and communities. This is addressed through the provision of culturally relevant health promotion/ disease prevention programs and services that focus on three targeted areas: Healthy Child Development; Mental Wellness; and Healthy Living, which support the healthy development of children and families, improve mental wellness outcomes and reduce the impact of chronic disease. Activities and priorities are established by recipients and are funded through contribution agreements.
2.1.1.1 Healthy Child Development sub-sub activity
The Healthy Child Development sub-sub-activity funds and supports a suite of community-based programs, services, initiatives and strategies that address greater risks and poorer health outcomes associated with First Nations and Inuit maternal, infant, child, and family health, including nutrition, early literacy and early learning and child care, physical health, oral health, and the promotion of First Nations and Inuit culture. Programming aims to improve health outcomes for First Nations and Inuit infants, children, youth, families and communities.
The Aboriginal Head Start On Reserve Program, within the Healthy Child Development sub-sub activity, as it pertains to the implementation of the Indigenous Early Learning and Child Care Framework, will have the ability to serve all First Nations children 0-6 and their families, living on and off reserve.
2.1.1.2 Mental Wellness sub-sub activity
The Mental Wellness sub-sub activity funds and supports a suite of community-based programs, services, initiatives and strategies that address greater risks and poorer health outcomes associated with the mental wellness of First Nations and Inuit, including members of landless bands (First Nation bands or Self-Governing First Nations registered in the Crown Indigenous Relations and Northern Affairs Canada (CIRNAC) Indian Registration System that do not have Reserve Land). Programming aims to contribute to the improved health status of First Nations and Inuit individuals, families, and communities through a range of culturally appropriate mental health and addictions programs and services, including prevention, early intervention, treatment and aftercare.
2.1.1.3 Healthy Living sub-sub activity
The Healthy Living sub-sub activity funds and supports a suite of culturally relevant community-based programs, services, initiatives and strategies that address greater risks and poorer health outcomes associated with chronic diseases and injuries among First Nations and Inuit individuals, families and communities. Programming aims to promote healthy behaviours through healthy eating; physical activity; food security; tobacco prevention, education, protection and cessation; chronic disease prevention; management and screening; and injury prevention.
2.2.1 Public Health Protection Sub-Activity
Health Protection is a core function of public health and is underpinned by surveillance supporting a population health approach. Within the FNIHB context, the fundamental objective of the Public Health Protection sub-activity is to prevent and/or mitigate human health risks associated with communicable diseases and exposure to hazards within the natural and built environments. This is accomplished through a range of activities at the individual, community and population levels including: provision of health services to prevent, manage and control communicable diseases and help assure the safety of food, water and living environments; promotion and education efforts to encourage healthy behaviours; research to identify and reduce environmental health risks; strengthening community capacity to take greater control over public health protection; and collaboration with partners to address the determinants of health, many of which are beyond the direct control of the public health system.
2.2.1.1 Communicable Disease Control and Management sub-sub activity
Communicable Disease Control and Management sub-sub activity is a core component of public health and is of particular concern in on-reserve First Nations communities and Inuit communities where the burden of communicable disease is higher than it is for other Canadians. This sub-sub activity supports a range of programs and initiatives to reduce the incidence, spread and human health effects of communicable diseases, in collaboration with other jurisdictions. Programming is delivered primarily through contribution agreements and focuses on vaccine preventable diseases (e.g. Varicella), blood borne diseases and sexually transmitted infections (e.g. HIV/AIDS), respiratory infections (e.g. tuberculosis), and communicable disease emergencies (e.g. pandemic influenza, COVID-19). Specific activities include public health measures to: identify risks (e.g. surveillance, reporting); prevent, treat and control cases and outbreaks of communicable diseases (e.g. immunization, screening, directly observed therapy); promote public education and awareness to encourage healthy practices; and strengthen community capacity (e.g. pandemic plans). A number of these activities are closely linked with those undertaken in the environmental health sub-sub activity, as they relate to waterborne, foodborne and zoonotic infectious diseases. Communicable disease control and management activities are targeted to on-reserve First Nations, with some support to address tuberculosis and other communicable diseases such as COVID-19 in First Nations and Inuit communities in Nunavut and the Northwest Territories.
2.2.1.2 Environmental Health sub-sub activity
Environmental Health sub-sub activity is a core component of public health protection. The objective of this sub-sub activity is to identify, mitigate and/or prevent human health risks associated with exposure to hazards within the natural and built environments. This is accomplished through the provision of environmental public health services; community capacity building activities; surveillance and research; and collaboration with partners to address the determinants of health. Programming is delivered directly by FNIHB and through Contribution agreements. Environmental public health programming is directed to First Nations communities south of 60° and addresses areas such as climate change, drinking water, wastewater, solid waste disposal, food safety, housing, facilities, and environmental aspects of emergency preparedness and response and communicable disease control. Specific activities include public education, sharing networks to support community-level decision making, training, and environmental public health assessments (e.g. public health inspections; investigations, monitoring and surveillance; infrastructure plan reviews; and the provision of advice and recommendations). North of 60°, responsibility for environmental public health programming has been transferred to territorial governments, FNIHB — Northern Region or First Nations and Inuit control as part of land-claims settlements. Environmental health research programming is directed to First Nations communities south of 60° and in some cases to Inuit and First Nations north of 60̊°. It includes community-based and participatory research on trends and impacts of environmental factors (e.g. contaminants, climate change) on the determinants of health (e.g. biophysical, social, cultural, spiritual).
2.3.1 Primary Care Sub-Activity
The Primary Care sub-activity is a coordinated system of health services required to maintain health and treat illness and is the first point of individual contact by First Nations and Inuit with the health system at the reserve/community level. Primary care is delivered by a collaborative health care team, predominately nurse led, providing a set of integrated and accessible health care services that include assessment, diagnostic, curative, rehabilitative, supportive and palliative/end-of-life care. It is where health promotion and disease prevention actions are directed towards individuals/families in the course of provision of care. The identification of cases requiring complex care, the coordination and/or integration of care, and timely referral to appropriate provincial/territorial secondary and tertiary levels of care outside the community are also essential elements of primary care. Primary care services are provided directly to First Nations and Inuit communities or through contribution agreements in locations where these services are not provided by provincial/territorial health systems and are necessary to ensure that First Nation and Inuit individuals and communities have access to the full range of health services as other provincial/territorial residents in similar geographic locations. Primary care services (including medical travel) are funded through contribution agreements with the Government of Northwest Territories until the end of 2024-25, and the Government of Nunavut until the end of 2025-26, for the benefit of Inuit and First Nations residents of the Northwest Territories and Nunavut, respectively, while a long term solution is being developed.
2.3.1.1 Clinical and Client Care sub-sub activity
The Clinical and Client Care sub-sub activity consists of essential health care services directed towards First Nations and Inuit individuals, living primarily in remote and isolated communities, that enable them to receive the clinical care they need in their home communities. It is provided either directly or through funding agreements with First Nation Bands or Tribal Councils in locations where these services are not provided by provincial/territorial health systems. It is also provided until the end of 2024-25 and the end of 2025-26 through funding agreements with the Governments of Northwest Territories and Nunavut, respectively, to support increased health care costs (including medical travel costs, fixed and variable air ambulance services costs, and the cost of administrating medical travel, while a long term solution is being developed). Clinical and Client Care is the first point of individual contact with the health system and is delivered by a collaborative health care team, predominantly nurse led, providing integrated and accessible assessment, diagnostic and curative services for urgent and non-urgent care. The continuum of Clinical and Client Care is inclusive of health promotion and disease prevention at the client/ family level in the course of treatment as well as the coordination and integration of care and referral to appropriate provincial and territorial secondary and tertiary levels of care outside the community. Physician visits, ambulatory and emergency services, and hospital in-patient care, are components of Clinical and Client Care services provided in some First Nations communities and supported through medical travel to ensure Inuit and First Nations residents in Nunavut and the Northwest Territories have access to these services.
2.3.1.2 Home and Community Care sub-sub activity
The Home and Community Care sub-sub activity is a coordinated system of health care services that enable First Nations and Inuit people of all ages with disabilities, chronic or acute illnesses and the elderly to receive the care they need in their homes and communities. It is provided primarily through contribution agreements with First Nation and Inuit communities and Territorial governments and strives to be equal to home and community care services offered to other Canadian residents in similar geographical areas. Home and Community Care is delivered primarily by home care registered nurses and trained and certified personal care workers. Service delivery is based on assessed need and follows a case management process. Essential service elements include client assessment; home care nursing; case management; home support (personal care and home management); in-home respite; linkages and referral, as needed, to other health and social services; provision of and access to specialized medical equipment and supplies for care; and a system of record keeping and data collection. Additional supportive services may also be provided, depending on the needs of the communities and funding availability. Supportive services may include, but are not limited to: rehabilitation and other therapies; adult day care; meal programs; in-home mental health; in-home palliative care; and specialized health promotion, wellness and fitness.
3. Legal and Policy Authority
The following legal and policy authorities support the Primary Health Care Authority and are grouped by their respective sub-sub program, where required:
- [DECISION – TBC]
- Addressing Unique Medical Travel Cost Pressures in Nunavut (2022)
- Funding for the Territorial Health Investment Fund and to Address Unique Medical Travel Cost Pressures in Nunavut (2021)
- COVID Emergency Response Act 2020
- Department of Indigenous Services Act, S.C. (2019)
- Department of Health Act 1996
- The Indian Health Policy (1979)
Health Promotion and Disease Prevention sub-activity
- Renewal of Federal Aboriginal Health Programs, April 2010
- Targeted and Immediate Action on Lung and Neurological Diseases, TB Submission, October 1st, 2009
- First Nations and Inuit Contribution Authorities Renewal Initiative, March and June 2005
- Follow-up to the Special Meeting of First Ministers and Aboriginal Leaders (September 2004), Approved-in-Principle, April 2005, and 2005 Federal Budget announcement
Healthy Child Development
- Addressing Anti-Indigenous Racism in Canada's Health Systems Memorandum to Cabinet, June 2021
- Implementation of the Federal Response to Jordan's Principle TB, March 12, 2009
- Enhancing Early Learning and Child Care (ELCC) for First Nations Children Living on Reserve and Working Towards the First Phase of a Single Window, October 2005
- First Nations and Inuit Dental Health, October 2003
- Early Childhood Development (Aboriginal Head Start On-Reserve and Off-Reserve, Fetal Alcohol Syndrome/Fetal Alcohol Effects, Early Childhood Development Capacity Building), September 2002
- Canada Prenatal Nutrition Program, Federal Budget announcement, February 1999
- Aboriginal Head Start On-Reserve, June 1998
- Brighter Futures June 1992
- Indigenous ELCC Framework
Mental Wellness
- Distinctions-Based Mental Health and Wellness Strategy Memorandum to Cabinet, December 2020
- Indian Residential Schools Settlement Agreement, Treasury Board decision, October 2003
- First Nations and Inuit Community Programs Class Contribution, March 2005
- First Nations and Inuit Health Governance and Infrastructure Support Class Contribution, March 2005
- Canada's Drug Strategy Renewed October 2003
- Building Healthy Communities (Mental Health Crisis Management Program, Solvent Abuse Early Intervention Program, Home Nursing), June 1994
- National Native Alcohol and Drug Abuse Program, March 1982
Healthy Living
- Nutrition North Canada: Funding to expand Nutrition North Canada Program to support all northern isolated communities, TB September 2016
- Upstream renewal, Aboriginal Diabetes Initiative, TB 2015
- Nutrition North Canada: Operation of Nutrition North Canada, a new northern healthy food subsidy program and its associated nutrition promotion/education initiatives, TB September 2010
- Nutrition North Canada: Renewal of the Food Mail Program – Towards a Renewed Northern Healthy Food Subsidy Program, TB May 13, 2010
- Food Safety and Nutrition Quality Program, TB Fall 1999
- Refocusing the Federal Tobacco Control Strategy 2012-2013 to 2016-2017 (and extended until 2017-2018)
Public Health Protection sub-activity
Communicable Disease Control and Management
- Addressing HIV/AIDS in Canada, November 2004
- Investing Upstream to Improve the Health of First Nations, January 2003
- Sustainability of First Nations and Inuit Health System ("First Nations Immunization Strategy"), August 2003
- Federal Initiative on HIV/AIDS
- Preparedness for avian and pandemic influenza
- Avian Influenza and Pandemic Influenza TB, October 5, 2006
- Canadian Strategy on HIV/AIDS, March 1998
- National AIDS Strategy for 1993-1994 to 1997-1998, Phase II, March 1993
- National AIDS Strategy for 1988-1989 to 1992-1993, Phase I, May 1988
- National AIDS Strategy for 1986-1987 to 1990-1991, April 1986
- Toward a Pan-Canadian Public Health System October 2004
- National Tuberculosis Elimination Strategy
- West Nile Virus program (now Environmental Communicable Disease Control) February 2004
Environmental Health
- Budget 2016 Green Investments – Funding for Health Canada (2016-2017 & 2017-2018) TB April 14, 2016
- Budget 2016 and Budget 2017 – Climate Change
- Budget 2010 (included a two-year extension of First Nations Water and Wastewater Action Plan (FNWWAP) at current funding levels)
- National Lung Health Framework 2009
- Implementation of the First Nations Water and Wastewater Action Plan, TB April 30, 2008
- Implementation of the Adaptation Theme in Support of Canada's Clean Air Agenda, TB April 30, 2008
- Standing Senate Committee on Aboriginal Peoples, 2007
- Standing Committee on Public Accounts, November 2006 (National Strategy to Address Mould in First Nations Communities)
- Clean Air Regulatory Agenda, TB October 12, 2006
- Office of the Auditor General's Report, May 2006 (Mould in on-reserve housing)
- Report of the Commissioner of the Environment and Sustainable Development, September 2005
- Implementation of the First Nations Water Management Strategy, August 2003
- Office of the Auditor General's Report, April 2003 (Federal government support to First Nations – Housing on reserve)
- Federal Water Quality Management Framework, February 2003
- Implementation of an action plan to protect human health from environmental contaminants TB April 3, 2008
- First Nations Biomonitoring Initiative
- Environmental Health Guide for Canadians Climate Change and Health Adaptation in Northern/Inuit Communities
- Adapting Asthma Guidelines
- Determine Risks to Lung Health Associated with Indoor Air Quality Among First Nations and Inuit Communities
Primary Care sub-activity
- Support to Improve Health Care Sustainability in the Territories, January 2005
- Investing Upstream to Improve the Health of First Nations, January 2003
- Effective and Sustainable Health System for First Nations and Inuit (Nursing Strategy, Capital, Non-Insured Health Benefits, Health Integration Initiative), December 2002
- First Nations and Inuit Home and Community Care Program, June 1999
Clinical and Client Care
- Effective and Sustainable Health System for First Nations and Inuit (Nursing Strategy, Capital, Non-Insured Health Benefits, Health Integration Initiative), December 2002
Home and Community Care
- First Nations and Inuit Home and Community Care Program, June 1999
4. Eligible Recipients and Annual Maximum Amount Payable
The following classes of recipients are eligible for funding under the Primary Health Care Authority categories of contribution. The following table lists the different classes of eligible recipients by sub-activity and the annual maximum amount payable for each sub-sub activity for this AuthorityFootnote 2.
The annual amount for the Primary Health Care Authority for each recipient will not exceed the following dollar values listed in Table 1 of this document. These levels were arrived at by conducting a review of historical funding levels and expenditures as well as input from program managers of Headquarters and regional offices.
| Eligible Recipients | Health Promotion and Disease Prevention | Public Health Protection | Primary Care | |||||
|---|---|---|---|---|---|---|---|---|
| Healthy Child Development | Mental Wellness | Healthy Living | Communicable Disease Control and Management | Environmental Health | Clinical and Client Care | Home and Community Care | Management and Delivery of Hospital Services | |
| First Nations in CanadaTable note 1 (ie, Communities, Bands, District, Tribal Councils and Associations) | $6,000 | $6,000 | $6,000 | $2,000 | $2,000 | $8,000 | $8,000 | $20,000 |
| Inuit Associations, Councils and HamletsTable note 1 | $6,000 | $6,000 | $6,000 | $2,000 | $2,000 | $5,000 | $5,000 | N/A |
| Canadian National Indigenous Organizations | $5,000 | $5,000 | $5,000 | $8,000 | $2,000 | $2,000 | $2,000 | $2,000 |
| Non-governmental and voluntary associations and organizations, including non-profit corporations | $6,000 | $6,000 | $6,000 | $4,000 | $4,000 | $6,000 | $6,000 | $4,000 |
| Educational institutions, hospitals and treatment centres | $8,000 | $8,000 | $8,000 | $4,000 | $4,000 | $6,000 | $6,000 | $20,000 |
| Municipal, provincial and territorial governmentsTable note 1Table note 2 | $8,000 | $8,000 | $8,000 | $4,000 | $4,000 | $8,000 | $8,000 | $20,000 |
| Health Authorities and Health Agencies | $8,000 | $8,000 | $8,000 | $4,000 | $4,000 | $8,000 | $8,000 | $20,000 |
|
||||||||
| N/A: Inuit Associations, Councils and Hamlets are not eligible for the Management and Delivery of Hospital Services. | ||||||||
5. Eligible Expenditures
As a result of the unique and complex nature of FNIHB transfer payments, FNIHB will include a generic list of specific eligible key activities for each sub-sub activity which falls under the Primary Health Care Authority. See Appendix H-2. Generally, eligible expenditures will include administration of the programs, staff salaries and benefits, contracts related to program planning and delivery, staff travel, office supplies, accommodation, printing, staff training, operation and maintenance of health facilities, utilities such as broadband connectivity and telecommunications, minor equipment and furniture for eligible program activities. Other expenditures may be considered eligible based on program plans provided. These are subject to FNIHB review and approval. While these are the broad expenditure categories, considerations may be given to allow other expenditures related to cultural and traditional activities. However, each approved plan will describe the eligible activities to be undertaken and a clause which states that all expenditures must be related to the delivery of health programs and services as defined in the agreement.
6. Stacking Provisions
The maximum level (stacking limits) of total Canadian government funding (federal, provincial, territorial and municipal assistance for any one activity, initiative or project) for recipients will not exceed 100% of eligible expenditures. The stacking limits must be respected when assistance is provided.
Recipients of contribution agreements are required to disclose any other government funding received for the same activity, initiative or project. Based on the provision of financial statements, financial reports and contribution audits, Indigenous Services Canada establishes whether stacking has occurred and if funds provided need to be recovered.
7. Basis and Timing of Payment
Payments are based on the achievement of predetermined performance expectations or milestones and/or a risk based approach. In FNIHB specific context and in order to provide cash flow to the recipient for delivering ongoing health programs and services, advance payments will be issued following a cash flow requirement forecast established in the contribution agreement. This may include, but is not limited to: historical funding levels, per capita, population/geographic indices, and the cost to deliver programs.
The method to be used to determine the amount of a contribution is based on a review of the Program Plan, Multi-Year Work Plan or Health and Wellness Plan submitted, as well as historical funding levels and in some instances, historical actual expenditures incurred by the recipient for the same activity being funded. With the implementation of the Contribution Funding Framework, recipients can enter into a two (2) year planning process to develop a plan (Multi Year Work Plan or Health and Wellness Plan).
For the purposes of putting in place contribution agreements with the Governments of the Northwest Territories and Nunavut for Inuit and First Nations residents' medical travel and related costs until the end of 2024-25 and the end of 2025-26 respectively, the Department may, when it considers it appropriate, reimburse the Governments of the Northwest Territories and Nunavut for eligible expenses that the Recipient has incurred from the beginning of the first fiscal year (2023-24) to the date of execution of the contribution agreement with the Department within the same fiscal year. Eligible expenses may only be reimbursed following the submission of documentation to the satisfaction of the Department. Canada's reimbursement of pre-agreement eligible expenses will be subject to the parameters specified in both the Program Terms and Conditions and the contribution agreement.
8. Application Requirements
FNIHB offers a variety of consolidated contribution agreements to First Nations and Inuit recipients that vary in the level of control, flexibility, authority, reporting requirements and accountability. At a minimum, recipients have a Set funding agreement which offers no flexibility, recipients deliver the programs and services as set out (prescribed) by the Branch. First Nations and Inuit communities interested in having more control of their health programs and services can decide among different approaches based on their eligibility, interests, needs and capacity. It is at this time that a recipient undergoes a recipient readiness assessment for a more flexible funding approach. Recently the Branch has also implemented the Risk Tolerance Strategy and this is another layer of assessing the recipient.
FNIHB has established relationships with First Nations and Inuit communities and other institutions through formal agreements to work together to develop, sustain and enhance their health, well-being and capacity to design, deliver and manage their health programs and services. By assuming control of their health programs and services, First Nations and Inuit are in a better position to meet their basic health needs. The long-term relationship established with eligible recipients impacts on the nature of the application requirements as well as on the level of flexibility of the financial arrangements chosen by both parties.
First Nations and Inuit interested in having more control of their health programs and services, have access to various types of funding approaches based on the demonstration of their eligibility, interests, needs and capacity. Based on need and capacity a recipient enters into the following funding approaches Set, Fixed, Flexible or Block. Discussions between FNIHB and the eligible recipient are conducted to form a decision on the approach that is best for the recipient.
For initial contribution agreements, the recipient must provide:
- For First Nation Bands and/or Inuit organizations, or a group formally mandated by Band Council Resolution or other formal mandate: Legal Entity Address and Telephone Number, Band Contract Person and Title, Legal Quorum to sign an agreement and Number of Councillors
- For Corporations: Incorporating Documents (Articles of Incorporation or Letters Patents), By-laws
- Disclosure of any involvement of former public servants who are subject to the Conflict of Interest and Post-Employment Code for Public Office Holders or the Conflict of Interest and Post-Employment Code for the Public Service
Regardless of the funding approach, the following requirements will apply to all community-based contribution agreements:
- A mandate, as evidenced by a Band Council Resolution (BCR), or other formal mandate for initial agreements, upon renewal of agreements or for the addition of any new initiatives, as required by the program.
- A plan: The Health and Wellness Plan, Multi-Year Work Plan, or multi-year Program Plan is the Recipient's primary document that identifies the community's health needs, defines its capacity to respond, and outlines its programs and services to address health priorities. The Health and Wellness Plan has the additional requirements of identifying all available resources, describing how various services will be integrated, and indicating how success will be measured. The plan becomes the focus for establishing priorities, building capacity, and enhancing accountability for program delivery. Additional details on the planning process are included in Appendix H-1.
- Evidence of demonstrated capacity in areas such as financial and administrative experience to deliver the programs and services. Successful experience in the management of programs and finances does not necessarily have to be in the area of health; it can also be in such areas as education, social services, and economic development.
In the interest of promoting program coordination and avoiding reporting burden, FNIHB will support consolidation of the contribution agreement planning and reporting requirements among programs that are delivered under the same contribution agreement with different funding approaches. The consolidation of the contribution agreement planning and reporting requirements will be established based on the most flexible funding approach used by the recipient.
Renewal of Contribution Agreements
The decision to enter into subsequent contribution agreements will be based on:
- evidence that a Plan has been implemented and updated
- discussions between the FNIHB and the recipient to determine if the agreement will be renewed
- all required reports and audits
- risk assessment
FNIHB may sign agreements with eligible recipients in partnership with other Branches/Sectors of Indigenous Services Canada and/or other federal departments for the provision of health services, specific programs and/or Block-funded services. All other aspects of the terms and conditions will remain applicable under these agreements while trying to ensure seamless requirements between funders.
Redistribution of Funding
This may include funding agreements where the recipient can redistribute funding to other entities. In these situations, the Department and the recipient would agree that this method is the most effective delivery model and the recipient would be independent in the choice of those entities, with minimum guidance from the department while adhering to the terms and conditions of the funding agreement.
9. Due Diligence in Managing and Administering the Transfer Payment Guidelines
Indigenous Services Canada ensures that FNIHB has financial resources for the effective, management, administration, and contribution audit activities related to programs under these terms and conditions.
9.1 Performance Measurement Strategy
The Performance Measurement Strategy developed for this authority demonstrates the department's intention and capacity to measure performance against key results commitments on an ongoing basis (ongoing performance measurement) and periodically through program specific research projects. The performance measurement strategy covers:
- main activities of the program, and its clients or target populations
- expected results
- performance indicators
- data collection sources and methods
- responsibility and frequency for collection
- reporting method
Departmental systems, procedures and resources are in place to ensure due diligence in approving transfer payments, verifying eligibility and entitlement, and managing and administering the Contributions Program. As the manager responsible for the Primary Health Care Authority, the Assistant Deputy Minister or designated representative will ensure:
- recipients are provided with appropriate assistance, advice or expertise
- progress of approved projects is monitored
- public funds are being managed appropriately
Indigenous Services Canada has established a Transfer Payment Management Control Framework (MCF) that ensures due diligence in the establishment and administration of contribution agreements. In addition, FNIHB has policies, procedures, a contribution management system and training tools to support the management of all contribution agreements.
FNIHB uses standard agreements to serve as vehicles for the administration and management of First Nations and Inuit community health programs and resources. These agreements vary in terms of level of control, flexibility, authority and, reporting requirements as described in the applicable Performance Measurement Strategy (ies). These agreements define the funding mechanisms in order to meet the needs of the recipient while taking capacity into account.
| Expected Results | Performance Indicators |
|---|---|
| Primary health care programs and services that are responsive to the needs of First Nations and Inuit individuals, families and communities. | Immunization coverage rates for two and seven year old children living on-reserve |
| Percentage of on-reserve population receiving required Primary Care assessment and diagnostic, treatment, rehabilitative, supportive and palliative care services. | |
Number and percentage of individuals, families and communities receiving required preventive, screening, treatment and support services for community-based health promotion/disease prevention programs by type of service:
|
9.2 Intervention Policy
As a result of the unique relationship developed with the recipients receiving funding to deliver health programs and services, an intervention policy has been developed to provide a framework for responding to the difficulties encountered by recipients with the management and/or delivery of programs. The intervention policy provides a list of potential triggers or indicators of the need for intervention, including default of the terms of the funding agreement, health emergencies, failure to deliver health programs and services and administrative/managerial difficulties. When intervention is required, the policy stipulates that the level of intervention must be appropriate to the situation, as determined through discussion with the recipient. Intervention may lead to third party management or other remedial management activities. Indigenous Services Canada may sign agreements, either alone or jointly with other departments, in support of remedial management activities, including third party management agreements.
9.3 Reporting Requirements
The contribution agreement contains provisions that outline the financial and non-financial reporting required from recipients. The level and frequency of reporting will vary depending on the mode of delivery. For targeted programs, reporting and accountability requirements specified in the contribution agreement will be at a level and frequency that is appropriate to determine whether program specific delivery requirements have been met and if expenditures were made by the recipient in accordance with the terms of the agreement.
Where special, time-limited funding is made available for programs or services aimed at specific health issues, the contribution agreement will stipulate any additional conditions associated with the funding. Unless otherwise specified, special, time-limited funding must be spent only for the purpose for which such funding is provided.
Existing mechanisms will be utilized to ensure that adequate reporting relationships, policy directions and administrative processes are in place to support the implementation, monitoring, and risk management of the Transfer Payments to meet the accountability of the recipient, the Department and of the Minister.
Contribution agreements with municipal, provincial and territorial governments, health agencies and health authorities as well as international organizations, require adjustments to accountability requirements, in order to align with existing accountability structures and legal obligations of these organizations. These adjustments are intended to avoid duplication and facilitate integration. A summary table of the requirements for due diligence is presented in Appendix H-3.
10. Audit Framework
10.1 Contribution Audits
Risk-based contribution audits are conducted in accordance with the FNIHB Audit and Quality Assurance Framework. This framework presents the kind of audit activities that the Branch may conduct, the related roles and responsibilities and the approval process. Contribution Audits are carried out in accordance with an annual audit risk-based audit plan that covers audits to be conducted based on an evaluation of risks.
The operational risks considered are the probability that:
- First Nation and Inuit communities do not receive health programs and services for which they are entitled
- Program funds are not used for intended purposes or in non-conformance with the terms and conditions of the contribution agreement or that First Nations and Inuit internal control practices are inappropriate
- Program funds being used for personal profit
Indigenous Services Canada is responsible for determining whether recipients have complied with the terms and conditions applicable to the contributions. FNIHB can look at individual contribution agreements based on systematic risk assessment and intuitive risk assessment of program management when a problem is suspected, or when program internal controls have failed (e.g. financial and operational monitoring).
10.2 Program Audits
The Audit and Accountability Bureau (AAB) is responsible for conducting periodic audits of the internal management policies, practices and controls. The AAB audits are based on a reasonable assessment of operational risk, the priorities of departmental management and available resources.
A Risk Management Strategy to support the Primary Health Care Authority was developed which details the risk profile for each main component of this authority. A Risk Assessment Tool was also developed to standardize the risk. Audit plans include provision for the review of internal management policies, practices and controls over transfer payment programs, and determination of the adequacy of the departmental processes to track whether recipients have complied with the requirements of applicable contribution agreements.
11. Official Languages
Where a program supports activities that may be delivered to members of either official language community, access to services from the recipient shall be provided in both official languages where there is sufficient demand. In addition, FNIHB will ensure that the design and the delivery of programs respect the obligations of the Government of Canada as set out in Part VII of the Official Languages Act by ensuring that these projects provide benefits to all Indigenous Canadians, including French and English minority communities. FNIHB will ensure that it has the capacity to communicate with, and provide services to, members of the public in the official language of their choice. All communication with the public from FNIHB (, press releases, announcements) will be in accordance with the Official Languages Act.
12. Other Terms and Conditions
12.1 Intellectual Property
Copyright in any material created by the funded recipient as the result of a contribution agreement related to the delivery of health programs and services in First Nation or Inuit communities will vest in the recipient. The Minister shall be entitled to use, reproduce and translate any such copyright material for any government purpose and may share such materials with provincial or territorial governments for internal use only, subject to deletion of any personal or confidential information where required by law. The Minister shall not otherwise distribute or disclose any material outside of the federal government unless authorized by law or the recipient.
Where a funded project or activity involves or additionally includes the creation of studies, research, reports, communications or other media relating to Indigenous health or the development of knowledge relating to Indigenous health, copyright will again vest in the recipient. The Minister shall be entitled to use, reproduce and translate any such copyright material for any government purpose and may share such materials with provincial or territorial governments for internal use only, subject to deletion of any personal or confidential information where required by law. The Minister shall also be entitled, by way of cost-free and royalty-free license, to distribute or disclose such materials outside of the federal government to any party if the materials are non-confidential information under the agreement and where the distribution is for non-commercial purposes only. For confidential studies or reports, external distribution should only be in accordance with the consent of those whose rights are affected or in accordance with law.
12.2 Termination
Either party may terminate a contribution agreement without cause by giving the other party notice in writing in accordance with processes defined in the contribution agreement. A termination clause is included in each agreement. The Minister may terminate at any time within the course pursuant to the remedies on default section of the contribution agreement or for reasons of appropriation.
13. Non-Monetary Contributions
The Minister may contribute goods, assets or services (rather than funding) to the recipient for health purposes. Non-monetary contributions may be employed in cases where the process would be of greater advantage to both parties and will not undermine long term objectives to increase First Nations and Inuit control of the delivery of health programs and services. Non-monetary contributions may consist of any good, asset or service that is required for, or can be used by, the recipient for health purposes, and may include for Primary Health Care: (i) any medical equipment or assets (and repairs thereto) for use by a recipient or that supports other health programs funded or delivered by the Minister (ii) goods or services required by the recipient to implement programs supporting Jordan's Principle.
The Minister will use Vote 10 funds for all non-monetary contributions, including the contracting for and delivery of such contributions to the recipient's community or the location where the recipient delivers health programs and services. The Minister will follow all federal contracting laws and policies for the purchase of non-monetary contributions. The Minister will ensure that the Recipient receives non-monetary contributions on the condition that they be used for health purposes and may require reporting and may audit for this purpose.
14. Funding Approaches
The diversity of interests, needs and capacities of the recipients leads to the requirement for divergent methods of delivering health community programs and services. This requires adaptable vehicles for the administration and management of health programs and services, which vary in terms of level of control, flexibility, reporting requirements and accountability. FNIHB will be using the following types of funding approaches: Set, Fixed, Flexible or Block. The funding approach relevant to programs and services is defined in the program framework and is dependent on the capacity of the recipient to manage and deliver programs, the class of eligible recipient, and the nature of the program. The funding approaches are further described in Appendix H-1.
Appendix H-1: Funding approaches
Contribution agreements can be established by combining programs and services from the different authorities (Primary Health Care, Supplementary Health Benefits and Health Infrastructure Support). The funding approaches within these authorities can be applied in a way that best suits the needs and capacity of the recipients provided that the approach used is within the approved program and policy framework established for the Branch.
Programs or services that are aimed at specific health issues may receive special time-limited funding, and this funding will have to be accounted for separately, no matter which funding approach is used. Time limited and additional programs/services may also be considered to complement core programs.
Exceptions:
Project-based agreements
For contribution agreements which are not community-based, but support the improved capacity of First Nations and Inuit to take on the responsibility of program management and delivery of effective programs and services, recipients will need to meet the requirements as outlined in Table 2, but their plan will take the form of a project proposal, budget, forecast or equivalent planning documents.
Indian Residential Schools Resolution Health Support
All contributions under the Indian Residential Schools Resolution Health Support will use the Set and/or Fixed funding approach. Under these approaches, the Recipient must use the resources as they are set out in the contribution agreement. Funds may not be redirected from the Indian Residential Schools Resolution Health Support Program to any other programs, without the prior written approval of the Minister. This will ensure that funds earmarked for the Indian Residential Schools Resolution Health Support Program are not used for activities outside the mandate of the program. The Recipient will be required to track and account for funds received under the Indian Residential Schools Resolution Health Support separately from all other funds received from FNIHB, including those received under the Mental Wellness sub-sub activity of the Primary Health Care Authority, if applicable.
The following table provides an overview of the funding approaches that FNIHB will be using as well as the distinct differences and reporting requirements.
| Requirements | Set | Fixed | Flexible | Block |
|---|---|---|---|---|
| Planning | Recipient follows multi-year Program Plan. This plan will include: objectives, activities that will be delivered. | Recipient follows multi-year Program Plan. This plan will include: objectives, activities that will be delivered. | Recipient establishes Multi-Year Work Plan including a health management structure. This Plan will include a budgetary plan, key priorities, objectives and activities that will be delivered. | Recipient establishes a Health and Wellness Plan including a health management structure. The Health and Wellness Plan will include key priorities, objectives, activities, mandatory health programs and other programs and services, annual reporting requirements, as well as information on the provisions of the professional / program advisory functions where applicable.
Ability to redesign non-mandatory programs. Ability to foster integration initiatives with flexible approaches and intergovernmental arrangements. |
| Reallocation of Funds | Recipients able to reallocate funds within the same Budget Activity on written approval by the Minister within the fiscal year reporting period. | Recipients able to reallocate funds within the same Budget Activity. | Recipients able to reallocate funds in the same Program Authority. | Recipients able to reallocate funds across authorities (with the exception of specifically identified programs). |
| Financial Reporting | Final (year-end) financial reports. | Annual year-end audit report. | Annual year-end audit report. | Annual year-end audit report. |
| Annual Program Reporting | Annual Report to the Minister based on annual reporting guide. | Annual Report to the Minister based on annual reporting guide. | Annual Report to the Minister based on annual reporting guide. | Annual Report to the Minister based on annual reporting guide. |
| Unexpended Funds | No retention of surplus and no carry over of funds into the next fiscal year. | Recipient are able to retain any unexpended funding remaining at the expiry of the agreement provided that the obligations and objectives set out in the funding agreement are met and the recipient agrees to use the unexpended funding for purposes consistent with the program objectives or any other purpose accepted by the Minister. | Recipients are able to carry over program funding annually for the duration of their agreement. Upon termination the recipient must reimburse the government any unspent funds. | Recipients able to retain surpluses to reinvest in priorities. |
| Must ensure the provision of all mandatory programs. | ||||
Appendix H-2: Eligible activities
In addition to the eligible expenditures listed in Section 5, the following tables list additional examples of the eligible key activities that fall under the Primary Health Care Authority's sub-activities:
| Name of Sub-Sub Activity | Eligible Key Activities |
|---|---|
| Healthy Child Development | Eligible key activities include: pre-conception and reproductive health care and promotion; pre-natal care; management of labour and delivery and post-partum/natal care (in the case of midwifery services); nutrition; breastfeeding promotion; early literacy and early learning and child care; physical health; oral health promotion, prevention and treatment; oral health training; public awareness; outreach; public education; early identification/diagnosis of Fetal Alcohol Spectrum Disorder; services for children with special needs; capital (in the case of Aboriginal Head Start On-Reserve and midwifery services); capacity building; continuing education; home visiting/outreach; screening and assessment; case conferencing/case management; coordination of services; the promotion of First Nations and Inuit culture and language; and program support activities such as early childhood development. Funding also supports knowledge development and dissemination, research, monitoring and evaluation, public education and outreach, capacity building, program coordination, consultation, and other health promotion and disease prevention activities related to Healthy Child Development. |
| Mental Wellness | Eligible activities include: mental health promotion; mental illness, addictions, solvent abuse, and suicide prevention; early intervention; residential and out-patient addictions treatment; mental health crisis management; professional and para-professional mental health counselling; resolution health support services; cultural and/or Elder supports; aftercare; capital (for residential addictions treatment facilities); capacity building; continuing education; and program coordination. Funding also supports knowledge development and dissemination, research, monitoring and evaluation, public education and outreach, capacity building, program coordination, consultation, communication, and other health promotion and disease prevention activities related to Mental Wellness. |
| Healthy Living | Eligible activities include: healthy eating/nutrition; physical activity; food security; tobacco prevention, education, protection and cessation; chronic disease prevention; management and screening; injury prevention; capacity building; continuing education; public education; outreach; and promotion of healthy behaviours and supportive environments. Funding also supports knowledge development and dissemination, research, monitoring and evaluation, program coordination, consultation, and other health promotion and disease prevention activities related to Healthy Living. |
| Name of Sub-Sub Activity | Eligible Key Activities |
|---|---|
| Communicable Disease Control and Management | Provision of communicable disease control and management programming, including infection prevention and control, surveillance, assessment, screening, contact tracing, outbreak management, diagnosis, referral, treatment, preventive interventions (e.g. immunization), counselling and follow-up. Culturally appropriate health promotion and disease prevention activities, including public education, social marketing and communications. Community development and capacity building initiatives associated with program management and administration, including emergency planning and response; and professional and paraprofessional capacity building, including training, staff development and continuing professional education to obtain and maintain appropriate competencies. Purchase, maintenance, storage and distribution of equipment and supplies necessary to deliver services and programming, including biologics and therapeutics (e.g. vaccines, medications, etc.), cold chain management (e.g. biologics refrigerators), personal protective equipment, associated infrastructure (e.g. safe storage) and other items necessary for infection prevention and control. Development and maintenance of surveillance systems, information management systems, and data collection tools and systems. Funding also supports research, knowledge translation and dissemination, monitoring and evaluation and collaboration with provinces, health authorities and other organizations. |
| Environmental Health | Provision of environmental public health services in the areas of drinking water, wastewater, food safety, housing, solid waste disposal, and facilities inspections, and in the context of environmental communicable disease control (foodborne, waterborne, vectorborne) and emergency preparedness and response, and other emerging issues in the areas of environmental public health. This includes: inspections and investigations; sampling, testing, monitoring and reporting; reviews, from a public health perspective, of infrastructure project plans; risk assessments; advice and recommendations; and consultations. Environmental health research activities (e.g. in the areas of environmental contaminants, food safety, climate change, determinants of health), including: scientific, community-based, participatory research projects; development and implementation of surveillance and performance data collection tools and reporting mechanisms; and evaluation, surveillance, monitoring, laboratory and data analysis and reporting. Development and dissemination of research, public education and awareness materials, best practices, procedures, manuals and guidance documents. Community capacity building initiatives such as collaborative events, consultations and knowledge sharing activities; as well as hiring and training of community-based water monitors, and recruitment, training and skills development and retention initiatives for environmental public health staff and management. |
| Name of Sub-Sub Activity | Eligible Key Activities |
|---|---|
| Clinical and Client Care | The provision of urgent and non-urgent assessment, diagnostic, treatment, collaborations with provinces and territories and health authorities and other organisations, quality improvement initiatives, operation and maintenance of the health facility from which services are provided; administrative support services for clinical and client care; continuing education of staff to obtain and maintain competencies; pharmaceuticals, medical supplies and equipment to support service delivery; record keeping, data collection and management. Purchase, maintenance, storage and distribution of equipment, pharmaceutical and supplies necessary to deliver services and programming. Funding also supports knowledge development and dissemination, research, monitoring and evaluation. Until the end of 2024-25 and the end of 2025-26, to address increased health care costs related to medical travel for Inuit and First Nations residents of the Northwest Territories and Nunavut, respectively, and to enable ISC to provide medical travel funding to the Governments of the Northwest Territories and Nunavut for these residents while a long term solution is being developed (beyond 2024-25 and 2025-26), eligible activities also include activities and patient access to activities that normally fall within the domain of the territorial governments’ health units, including medical transportation, air ambulance and administration of medical travel for Inuit and First Nations residents of the Northwest Territories and Nunavut. |
| Management and Delivery of Hospital services
Management and continued operations and physicians services, staff salaries, staff and Board training, physical plant and utilities, staff housing, diagnostic and laboratory services, medical supplies and drugs, dental services, rehabilitation services, surgical services, medical services, patient support services, family medicine clinic, corporate services, patient record services; continuing education of staff to obtain and maintain competencies; administration; and governance. |
|
| Home and Community Care | Needs assessment and developmental projects while in planning, home and community care assessment, treatment, rehabilitative, supportive and palliative/end-of-life services including structured client assessment process, managed case process, home care nursing services, home support personal care services, provision of access to in-home respite care, and access to medical equipment and supplies); administrative support services for home and community care; continuing education of staff to obtain and maintain competencies; supplies and equipment to support service delivery; record keeping, data collection and management. Purchase, maintenance, storage and distribution of equipment and supplies necessary to deliver services and programming. Funding also supports knowledge development and dissemination, research, monitoring and evaluation. |
Appendix H-3: Summary of requirements for due diligence
| Set | Fixed | Flexible | Block | |
|---|---|---|---|---|
| Planning Requirements (At the beginning of each year of agreement) | ||||
| Program PlanFootnote 3 | Yes | Yes | No | No |
| Multi-Year Work Plan | No | No | Yes | No |
| Health and Wellness Plan | No | No | No | Yes |
| Reporting Requirements | ||||
| Auditor's Report | No | Yes (annual) | Yes (annual) | Yes (annual) |
| Balance Sheet | No | Yes (annual) | Yes (annual) | Yes (annual) |
| Combined Statement of Revenue, Expenditures and Accumulated Surplus | No | Yes (annual) | Yes (annual) | Yes (annual) |
| Financial Report on Health Program Expenditures | Yes (year end only) | No | No | No |
| Report on the Provision of Mandatory Programs | Yes (as required by authorities) | Yes (as required by authorities) | Yes (as required by authorities) | Yes (as required by authorities) |
| Annual Report to the Minister | No | No | No | Yes |
| Report on Program Activities (other than mandatory) | Yes | Yes | Yes | No |