A Review of Jordan's Principle
March 2019
Evaluation, Performance Measurement
and Review Branch
Audit and Evaluation Sector
PDF Version (552 Kb, 59 Pages)
Table of contents
- Acronyms
- Executive Summary
- 1. Background
- 2. Scope of Work
- 3. Case Studies Issues and Questions
- 4. Selected Case Studies
- 5. Methodology
- 6. Key Findings
- 7. What are the Key Strengths and Challenges, and what are the Lessons Learned?
- Appendix A: My Child, My Heart Case Report
- Appendix B: Choose Life Case Report
- Appendix C: Early Childhood Intervention Program Regina Case Report
Acronyms
| CDW |
Child Development Worker |
|---|---|
| CHRT |
Canadian Human Rights Tribunal |
| ECE |
Early Childhood Educators |
| ECIP |
Early Childhood Intervention Program |
| FNIHB |
First Nations and Inuit Health Branch |
| FTE |
Full-Time Equivalent |
| ISC |
Indigenous Services Canada |
| INAC |
Indigenous and Northern Affairs Canada |
| KOSSS |
Keewaytinook Okimakanak Secondary School Services |
| NAN |
Nishnawbe Aski Nation |
| OT |
Occupational Therapy |
| PT |
Physical Therapy |
| SLP |
Speech Language Pathologists |
| SSF |
Specialized Support Facilitators |
Executive Summary
Background and Methodology
Jordan's Principle originated in 2007, stemming from the inequities in services First Nations children were receiving on-reserve in comparison to their non-First Nation counterparts. Jordan's Principle includes a $382 million dollar commitment over three years (2016‑2019) on behalf of the Government of Canada to enable service coordination, service access resolution, data collection and capacity building to ensure that First Nations children, regardless of on- or off‑reserve status, receive equitable treatment and access to government funded services.
R.A. Malatest & Associates Ltd. was contracted to complete a Review of Jordan's Principle. The Review was not intended to be a full evaluation of Jordan's Principle, but rather, to identify how projects funded by Jordan's Principle were implemented in some communities, including the identification of challenges, successes and the lessons learned in those communities.
Completed in a compressed timeframe, the Review site visits occurred between August to September 2018, and the analysis and reporting took place from October to November 2018. Two of the three case studies assessed Jordan's Principle funding that was provided to expand and enhance pre-existing programming (i.e., My Child, My Heart, and the Early Childhood Intervention Program (ECIP), while one of the case studies reflected the experiences of an entirely new program (Choose Life). My Child, My Heart, provides case management of services to children 0-21 with severe needs, which includes the provisioning of services to their families as needed. ECIP was established in Saskatchewan in 1980 to provide services to children with developmental delays; Jordan's Principle funding allowed the extension of services from children aged 0 to 6 to children and youth aged 6 to 17. Choose Life projects were designed to address mental health and resilience issues among youth in northern Ontario, as this area has largely experienced a high rate of youth suicides in the past.
Case studies completed as part of the Review (My Child, My Heart; the Early Childhood Intervention Program; and Choose Life), included a review of available program documentation, a two to three day site visit to the program delivery location, a development of a community profile, and interviews and focus groups with program staff, stakeholders and parents. Findings from the Review are limited in that only a very small proportion of funded projects were examined, and short timelines meant administrative data was not available, project documentation was limited, and data collection was completed with stakeholders who were available at the time of the site visit.
Review Findings
Operating Context and Service Gaps
Projects that had existing infrastructure or were extensions of existing projects experienced fewer implementation challenges than did new projects. Generally, projects that were new lacked a solid understanding of program design, program theory (linking activities to outcomes), assessment and intake procedures, case management processes, assessment and measurement processes, and development of service plans. When located in rural or remote locations, programs also struggled with the availability of qualified and trained staff in the community and availability of other resources (training, referral service providers, etc.). Across all sites, the lack of funding for youth older than 17 years of age was noted as the major service gap.
Roles and Responsibilities
Roles and responsibilities among partner organizations or other community service providers were best documented in pre-existing programs. While relationships existed between the project and some primary partners, program design was not based on an extensive consultation with all stakeholders and/or service partners. Consultation and communication had occurred between the funded projects and other stakeholders, but such consultation was generally initiated by project staff during informal case management rather than as part of a formal communication/outreach strategy.
Service Delivery Similarity Across Funded Projects
Each of the five projects reviewed had considerable variation in program consultation, design, implementation and execution. Most had enhanced or aimed to enhance case management, most had introduced new program activities, all had some focus on providing parents supports (although it was limited), and all had introduced some new staff, while two used existing staff and support services.
Changes Under Jordan's Principle for Children Families
Jordan's Principle funding appeared to have positive outcomes for children and their families. Case study participants identified a range of outcomes such as a reduction of negative incidents among youth, improved school attendance, the ability for families to remain living on‑reserve, and improved supports for parents. More specifically, parents noted that of significant benefit was the: introduction of an active champion who helped assess and meet the needs of their children, positive child outcome from the supports provided (e.g. improved ability of their child to communicate their needs when they are non-verbal), and improved educational outcomes.
Jordan's Principle Contribution to Improved Service Coordination or Partnerships
Coordination of services was likely improved under Jordan's Principle, but for the projects that were visited, a high degree of service coordination was not observed (although relationships exist with referral agencies). As part of the program roll-out, programs undertook consultations with communities and service providers as to program objectives and elements; however, programs were not always designed in a stepwise manner (program coordination and consultation, funding for program design, and funding for program implementation).
Key Strengths
Generally all programs provided new funding to fill gaps in services and programs were designed to meet local/community need. Similarly, parents were provided with needed supports that were otherwise missing. An important strength of Jordan's Principle noted by stakeholders was the rapid and timely approval of funding (for families) and the high level of project approval.
Lessons Learned
Key lessons learned included:
- Program effectiveness was impacted by the operating time, the availability of resources to design and implement programming, and the availability of resources and staff to maintain programming.
- Programs require support in developing program theory to link program activities to intended outcomes. Further, programs require support in measuring and monitoring these outcomes.
- More guidance should be provided to programs to allow program implementation to occur in a stage wise approach that includes community consultation, program design and program roll-out.
- Capacity and infrastructure challenges can be addressed at a high level through "tool‑kits" and training.
1. Background
1.1 Overview
This report summarizes the key findings associated with the Review of Jordan's Principle, initiated by Indigenous Services Canada (ISC) in the summer of 2018. This Review is not intended to be a full evaluation, but rather, is intended to identify how Jordan's Principle was implemented in some communities, to identify challenges and successes, and provide some insights as to lessons learned in these communities. It should be emphasized that results cannot be generalized to all activities funded under Jordan's Principle, as the researchers were only able to conduct reviews of five projects in three different jurisdictions. Thus, given that there were hundreds of projects funded, the case studies represent only a fraction of all projects supported by Jordan's Principle.
1.2 Jordan's Principle
Jordan's Principle originated in 2007 stemming from a formal complaint on behalf of the First Nations Child and Family Caring Society and the Assembly of First Nations; this complaint was directed to the Canadian Human Rights Tribunal (CHRT) regarding the inequitable services First Nations children were receiving in comparison to their non-First Nation counterparts.
Jordan's Principle arose from the experience of Jordan River Anderson, a First Nations boy from Norway House Cree Nation in Manitoba. Jordan had severe medical issues, including a rare disorder, and was consequentially hospitalized from birth. Jordan passed away at the age of 5 before getting an opportunity to live in a medical foster home, as the provincial and federal government disputed who has financially responsibility for Jordan's care.
In order to resolve jurisdictional disputes involving the care of First Nations children, the House of Commons of Canada adopted a motionFootnote 1 in December 2007, called Jordan's Principle. This principle provides that "where a government service is available to all other children, but a jurisdictional dispute regarding services to a First Nations child arises between Canada, a province, a territory, or between government departments, the government department of first contact pays for the service and can seek reimbursement from other governments or department after the child has received the service."Footnote 2 This principle essentially seeks to prevent First Nations children from being denied essential public services or experiencing unreasonable delays in receiving such services.
On May 26, 2017, and amended on November 2, 2017, the CHRT issued a ruling that included an expanded definition of Jordan's Principle:
"[2] In recognition of Jordan, Jordan's Principle provides that where a government service is available to all other children, but a jurisdictional dispute regarding services to a First Nations child arises between Canada, a province, a territory, or between government departments, the government department of first contact pays for the service and can seek reimbursement from the other government or department after the child has received the service. It is a child-first principle meant to prevent First Nations children from being denied essential public services or experiencing delays in receiving them. On December 12, 2007, the House of Commons unanimously passed a motion that the government should immediately adopt a child-first principle, based on Jordan's Principle, to resolve jurisdictional disputes involving the care of First Nations children."
"[135]…Canada's definition and application of Jordan's Principle shall be based on the following key principles:
- Jordan's Principle is a child-first principle that applies equally to all First Nations children, whether resident on or off reserve. It is not limited to First Nations children with disabilities, or those with discrete short-term issues creating critical needs for health and social supports or affecting their activities of daily living.
- Jordan's Principle addresses the needs of First Nations children by ensuring there are no gaps in government services to them. It can address, for example, but is not limited to, gaps in such services as mental health, special education, dental, physical therapy, speech therapy, medical equipment and physiotherapy.
- When a government service, including a service assessment, is available to all other children, the government department of first contact will pay for the service to a First Nations child, without engaging in administrative case conferencing, policy review, service navigation or any other similar administrative procedure before the recommended service is approved and funding is provided. Canada may only engage in clinical case conferencing with professionals with relevant competence and training before the recommended service is approved and funding is provided to the extent that such consultations are reasonably necessary to determine the requestor's clinical needs. Where professionals with relevant competence and training are already involved in a First Nations child's case, Canada will consult those professionals and will only involve other professionals to the extent that those professionals already involved cannot provide the necessary clinical information. Canada may also consult with the family, First Nation community or service providers to fund services within the timeframes specified in paragraphs 135(2)(A)(ii) and 135(2)(A)(ii.1) where the service is available, and will make every reasonable effort to ensure funding is provided as close to those timeframes where the service is not available. After the recommended service is approved and funding is provided, the government department of first contact can seek reimbursement from another department/government;
- When a government service, including a service assessment, is not necessarily available to all other children or is beyond the normative standard of care, the government department of first contact will still evaluate the individual needs of the child to determine if the requested service should be provided to ensure substantive equality in the provision of services to the child, to ensure culturally appropriate services to the child and/or to safeguard the best interests of the child. Where such services are to be provided, the government department of first contact will pay for the provision of the services to the First Nations child, without engaging in administrative case conferencing, policy review, service navigation or any other similar administrative procedure before the recommended service is approved and funding is provided. Clinical case conferencing may be undertaken only for the purpose described in paragraph 135(1)(B)(iii). Canada may also consult with the family, First Nation community or service providers to fund services within the timeframes specified in paragraphs 135(2)(A)(ii) and 135(2)(A)(ii.1) where the service is available, and will make every reasonable effort to ensure funding is provided as close to those timeframes where the service is not available. After the recommended service is provided, the government department of first contact can seek reimbursement from another department/government.
- While Jordan's Principle can apply to jurisdictional disputes between governments (i.e., between federal, provincial or territorial governments) and to jurisdictional disputes between departments within the same government, a dispute amongst government departments or between governments is not a necessary requirement for the application of Jordan's Principle."Footnote 3
Jordan's Principle is designed to ensure that First Nations children, regardless of on- or off-reserve status, receive equitable treatment and access to government funded services. Some of the service areas funded under Jordan's Principle include:
- mental health;
- dental care;
- special education;
- physical therapy;
- speech therapy;
- medical equipment; and
- physiotherapy.
Jordan's Principle aims to implement the services and support to assist children with complex medical conditions, as well as their families. This ranges from mobility devices for children with health conditions to mental health/wellness programs designed to address mental health issues among First Nations youth. In addition to providing supports to children, a number of projects funded under Jordan's Principle also provide counselling and case management supports to parents or caregivers.
1.3 Jordan's Principle Implementation
The implementation of Jordan's Principle included a $382 million dollar commitment over three years (2016-2019) on behalf of the Government of Canada to enable:
- Service Coordination: Fund external organizations in order to provide supports where identified (gaps);
- Service Access Resolution Fund: Allocation of funds for Health Canada and Indigenous Northern Affairs Canada (INAC) to meet identified gaps;
- Data Collection: Collect and analyze service and financial data; and
- Capacity: Resources to ensure adequate human resource capacity regarding implementation.
Based on the CHRT's ruling, for most cases ISC is required to process requests for services within 12 to 48 hours. The timeframes for processing requests are outlined below.
Requests for a child or children in the same family or with the same guardian:
- Urgent requests (the child's current health or safety is a concern) are processed within 12 hours of receiving all necessary information; and
- All other requests are processed within 48 hours of receiving all necessary information if we do not have enough information to confirm the type of product, service or support the child needs, more time may be necessary to get this information; however, if the child requires an assessment of their need(s), this can be paid for immediately under Jordan's Principle.
Requests for a group of children from multiple families or guardians:
- Urgent requests are processed within 48 hours of receiving all necessary information; and
- All other requests are processed within one week of receiving all necessary information.
Requests that are approved under Jordan's Principle are managed by ISC in one of two ways:
- Where possible, ISC arrange for the products, services or supports to be provided directly to the child, or children. In these situations, there is no cost to the family, guardian, child or authorized representative and reimbursement is arranged directly with the service provider or vendor.
- If the family, guardian, child or authorized representative has already paid for the approved product, service or support, then reimbursement of these expenses is provided.Footnote 4
From the Jordan's Principle Government of Canada website, it is indicated that more than 165,000 requestsFootnote 5 had been approved by the federal government during the period from 2016 to September 2018. Furthermore, information supplied by Health Canada suggests that the approval rate for such requests was very high – at approximately 99 percent approval.
2. Scope of Work
2.1 Overview
For the purposes of this Review, case studies were selected with respect to the services coordination component, which included funding to specific projects designed to assist children/families. As part of the Review, interviews and focus groups were also held with parents to discuss how they had accessed Jordan's Principle funding and the impacts of such funding for themselves and their children.
As noted previously, R.A. Malatest & Associates Ltd. was contracted to complete a review of Jordan's Principle, which included examination of some program documentation (when available), but primarily relied on a case study methodology, which included site visits to five (5) funded projects in three jurisdictions across Canada (Ontario, Manitoba, Saskatchewan). The case study locations were identified by ISC although the specific projects assessed were developed in consultation with the project sponsors.
It should be emphasized that this Review was completed in a very compressed timeframe. The project was approved in July 2018, and site visits occurred in August to September 2018. Analysis and reporting took place in October to November 2018. The Review was also hampered by limited program documentation, and there was no program administrative data tracking either outputs or outcomes. Nevertheless, the results should be viewed with confidence given the in-depth approach taken with respect to the completion of each case study as well as the commonality of findings observed as part of this Review.
2.2 Purpose
The purpose of the Review was to assess the high level implementation of projects funded under Jordan's Principle, and to identify challenges and successes and, where appropriate, highlight outcomes achieved in the selected case studies.
In completing this Review, the research was guided by the following objectives, including to:
- Assess best practices;
- Include lessons learned; and
- Identify service delivery approaches that could be generalized.
In order to gain a broad understanding of the impact of project funding under Jordan's Principle, there were a diverse set of sites selected for the case study review. The models selected included expansion of pre-existing programs, sites which introduced entirely new programs/services, as well as projects which provided services on a province-wide basis. The actual sites visited are described in greater detail in Section 4 of this report.
The research activities completed as part of this Review included an examination of documentation, as well as interviews/focus groups with program staff, service partners, stakeholders and parents. As noted previously, while the focus of the Review was to assess "projects" funded under the service coordination initiative, the research team also collected considerable data pertaining to parental experiences with Jordan's Principle in terms of receipt of funding to support themselves or their children (i.e. respite, assistive devices, other). Additional information as to the specific research activities completed can be found in Section 5 of this report (Methodology).
3. Case Studies Issues and Questions
The Review of Jordan's Principle was designed to provide insights on a number of key issues and questions. These issues include:
- What is the overall context in which the delivery models are operating (in relation to Jordan's Principle)?
- How are these models being implemented?
- What gaps in service delivery need to be addressed?
- What are the roles and responsibilities of stakeholders and partners, and how do they work together?
- In what way is service delivery similar or different among the models?
- What has changed under Jordan's Principle?
- To what extent has Jordan's Principle contributed to the creation/improvement of partnerships, processes and service coordination through these initiatives?
- What are some key strengths and challenges, and what lessons learned can be taken to inform the longer term planning process?
- What are the resource requirements for each model? [not addressed in this report]
- What data collection tools and mechanisms are in place to support the identification and reporting, monitoring of services, both new and existing? [not addressed in this report]
It should be noted that due to the research methods used (case studies) and the limited availability of data; it was not possible to provide answers or insights to the last two research issues (resource requirements, data collection and monitoring tools).
4. Selected Case Studies
As noted previously, the case studies identified for inclusion in this Review were selected on the basis of different criteria. While two of the three case studies represented the "extension" of existing programming, one of the case study initiatives reflected the experiences of entirely new projects. Furthermore, the inclusion of the Early Childhood Intervention Program (ECIP) in Saskatchewan provided some insights as to funding for a province wide initiative. Additional details for each case study are provided below. In addition, detailed findings for each of the three case studies are included in the appendices to this report.
4.1 My Child, My Heart (Manitoba)
The My Child, My Heart case study (see Appendix A) represents funding provided for a pre-existing program that received funding to support continuation and enhancement of the programming. The program was initiated in 2015 as a pilot project. The project is located in the Pinaymootang First Nation in northern Manitoba. The project includes intensive case management services provided to children aged 0-21 irrespective of on/off‑reserve status, as well as their families as needed.
The two core goals of the My Child, My Heart project were as follows:
- Service provision for children; and
- Development of practice standards and guidelines for First Nations implementation of Jordan's Principle in Manitoba.
4.2 Choose Life (North Western Ontario, Three Projects)
The Choose Life case study (see Appendix B) represents funding provided to projects that did not exist prior to Jordan's Principle. In the case of Choose Life, three projects were selected for Review out of more than 122 Choose Life projects that had been funded under Jordan's Principle in the Nishnawbe Aski Nation (NAN). Many of these projects were designed to address mental health and youth resilience issues, as the region had experienced a high rate of youth suicides in the past. Many of the projects included funding for land-based programs that served to build youth self‑esteem, cultural affiliation and self-worth.
In discussion with the Choose Life co-ordinators, it was noted that many of the projects were "new", and were only funded in fiscal year 2016-17 or fiscal year 2017-18 with funding ending in March 2019. As noted previously, the selected projects were designed to address youth mental health/crisis issues.
As part of the case study, three projects were examined including:
- Keewaytinook Okimakanak Secondary School Services (KOSSS) - Thunder Bay;
- KOSSS – Sioux Lookout (Home Support Workers); and
- Lac Seul (Land Based Program).
4.3 Early Childhood Intervention Program (Regina Saskatchewan)
The ECIP (see Appendix C) was established in Saskatchewan in 1980 to provide services to children with developmental delays (i.e. genetic, environmental, medical etc.). ECIPs are primarily funded by the Saskatchewan Ministry of Education, although ECIPs typically receive additional funding. In Saskatchewan, ECIPs had received funding from various federal departments (Health Canada, First Nation and Inuit Health Branch (FNIHB), INAC, ISC) to provide services to on-reserve First Nation youth aged 0-6. However, under Jordan's Principle, ECIPs in Saskatchewan applied and received funding to expand services to include First Nation youth (both on- and off‑reserve) aged 6 to 17 (and in some cases aged 21).
The core services provided by ECIPs include the following:
- Family Support (via Jordan's Principle application support);
- Case Coordination and Transition Support;
- Community Development and Partnerships; and
- Referrals.
It should be noted that while ECIPs generally provide the same services, the focus of the case study was the Regina ECIP, although data was collected as to the program activities undertaken in two other ECIPs (Children North – La Ronge, and Northeast) as part of Jordan's Principle funding.
5. Methodology
5.1 Methods
The Review included an examination of documentation provided by ISC, online review of the programs/services offered in each case study community, and a site visit to the program delivery location.
In advance of each site visit, a community site visit profile was developed. The profile provided important background information about the community as well as the programs/services that were available in each community.
Staff from Malatest arranged visits to each community. Generally, each case study included three days "onsite" as well as time to travel to/from the location. In coordinating visits to each community, it was mentioned that the research team would like to meet with program staff, service providers, other stakeholders and parents as appropriate.
The sites visited and data collection that occurred is detailed in Table 1.
| Site/Activity | My Child, My Heart | Choose Life | ECIP Regina |
|---|---|---|---|
| Community | Pinaymootang First Nation, Manitoba |
|
Regina, Saskatchewan |
| Dates | Aug 20-22, 2018 | Sep 19-21, 2018 | Sep 24-26, 2018 |
| Consultations |
Program Staff/ coordinator (4) |
Thunder Bay – NAN
Thunder Bay – KOSSS
Sioux Lookout – KOSSS
Lac Seul
|
ECIP Coordinators (3)
ECIP Regina staff (4)
|
5.2 Research limitations
It should be noted that this Review had several limitations. These limitations include:
- Short timelines: The Review was completed on a short timeline. The project started in July 2018, site visits occurred in August to September 2018, and final reporting occurred in October to November 2018. As a result of this compressed schedule, it was not possible to conduct an in-depth examination of administrative data (which was not available), nor was it possible to obtain additional data about the sites. Scheduling issues also limited the extent to which staff, other stakeholders and parents could participate in the study.
- Limited access to reports/documentation: While the research team was provided with limited documentation for the selected case study projects, there were other important documents that were not provided to the team. Among these included the annual reports submitted by each project that would have provided additional information as to services provided and children served.
- Qualitative focus: Case studies by definition tend to provide detailed contextual information, however, findings from case studies are difficult to "generalize" to all projects. This is problematic in terms of estimating the cost of service provisions as well as other indicators such as child development, school transition, and/or other metrics associated with improved child/family well-being.
- Possible Selection Bias: It should be noted that the project coordinators selected/identified the appropriate staff, stakeholders and parents who were interviewed as part of this Review. In this context, it is possible that individuals selected were purposely chosen for their positive support of the program.
6. Key Findings
Key findings in this section are presented under the key research questions as previously described in Section 3 of this report. Findings have been generalized across the various case study sites visited and represent the Research Team's interpretation of findings.
6.1 What is the overall context in which the delivery models are operating (in relation to Jordan's Principle)?
Overall, it was found that projects that had existing infrastructure or were extensions of existing projects (My Child, My Heart, ECIP Regina) experienced fewer implementation challenges than did "new" projects (Choose Life projects).
In general, it was found that the new projects lacked:
- Understanding of program design process;
- Understanding of how to link program activities with desired outcomes;
- Understanding of appropriate assessment and intake procedures in mental health;
- Availability of qualified and trained staff in the community;
- Time to develop relationships with other community service providers;
- Development of case management models;
- Community isolation impacts resource availability; and
- Two year funding window was insufficient for program design and implementation.
In addition, it was found that in the more isolated communities, there was a general lack of clinical and professional supports (mental health workers, other health professionals) that impeded the ability of projects to deliver programs and services. Furthermore, project stakeholders noted that the two year funding window for new projects did not allow for sufficient time to design, implement and modify programs to meet community and client needs.
It is important to acknowledge that given the CHRT's ruling that applications be processed within 12 to 48 hours and that service gaps be quickly addressed by the federal government, it is not unexpected that new projects that did not have pre-existing health services infrastructure would also not have comprehensive design and delivery approaches. It is expected that with funding stability, new projects and programs would have more time and capacity to develop their approaches and this would help ensure a smoother roll-out and implementation.
6.2 How are these models being implemented?
As noted previously, for those programs/projects in which there was a pre-existing program or infrastructure, program roll-out and implementation proceeded much more smoothly than was the case in projects that were being developed "from scratch".
In general, project coordinators noted that they did spend time talking to other stakeholders and First Nation communities about the proposed program/project, but the level of consultation varied on a project by project basis.
For newly designed projects or programs (i.e. Choose Life), it was found that program implementation lacked proper program design and implementation structures. For example, due to the tight funding window, it was noted that there was limited or no time to undertake a community analysis, do proper "gap identification" and develop a proper service plan. For new programs, such programs were often introduced without a program logic model (relating how inputs and activates would support desired outcomes), nor were community service maps generally developed (that would identify who could provide what services in each community). Furthermore, new programs were generally launched in their entirety, but could have benefitted from an approach that made use of pilots and/or phased implementation.
Program coordinators also noted that they received very little support or guidance from Health Canada. While Health Canada staff did work with the program coordinators to help ensure that submitted application would eventually result in a funded project (particularly in Choose Life), they offered little assistance in terms of providing advice/guidance as to the steps that should be taken to introduce new health programming at the community level. As noted, given the rapid roll‑out of programming to meet the CHRT requirements, in many cases, there was likely not enough time to provide sufficient support for new programming.
This was a classic "learn as you go approach"; I wish that someone could have given us more direction or help in terms of setting up this program and making us aware of what "we did not know"
6.3 What gaps in service delivery need to be addressed?
Across the various sites visited, a common theme that emerged was the desire to see programming for youth extended beyond the current guidelines of 0 to 17 years of age. As one stakeholder noted:
The issues faced by an individual do not disappear when they turn 18 years of age.
While some projects did make allowances to provide supports to individuals up to the age of 21, it was felt that more guidance/funding should be provided to either support older individuals (to age 24 or even age 29), or provide transitional supports to such individuals. In addition, it was noted that some individuals had already "aged out" of Jordan's Principle funding having spent their entire youth without appropriate supports and services.
While both program staff and stakeholders noted that the Jordan's Principle funding had allowed for the provision of programs and services, not all children/families were actually receiving required services. This did not reflect a program issue, but rather, difficulty in securing appropriate qualified staff in rural/remote regions (Psychiatrists, Speech Language Pathologists (SLPs), and Occupational Therapists etc.). Additionally, with My Child, My Heart, program staff acknowledged that it takes time for children with developmental delays to be identified and for the parents to then accept that their child requires additional supports.
6.4 What are the roles and responsibilities of stakeholders and partners, and how do they work together?
As part of Jordan's Principle, the degree to which project sponsors engaged in community/service partner outreach to identify program gaps and possible service delivery options varied. Existing programs appeared more aware of other service providers and had more formalized approaches to case management. In new programs, stakeholders and project proponents noted that such consultations did occur, however, it appears that consultations were not comprehensive nor did they formally involve all service partners, in program design/administration.
Thus for new programs, it did not appear that the roles/responsibilities of all service partners were identified and documented. While relationships existed between the project and some primary partners (i.e. KOSSS Sioux Lookout and local school board), program design was not based on an extensive consultation with all stakeholders and/or service partners. For example, there was no evidence of comprehensive service coordination given that the projects visited did not developed a "community service map" (i.e. identify what social/health services already existed in the community), nor was there evidence of agreements (Memoranda of Understanding, other) between the funded projects and other service coordinators. In fact, in the ECIP case study, it was noted that Health Canada may have actually funded two very similar projects in the same community (i.e. ECIP was funded to hire Speech Language Pathologist to provide services to on-/off‑reserve First Nation youth, and a nearby First Nation Band was also provided funding to hire a Speech Language Pathologist to provide services to some of the same children).
It was noted that consultation and communication did occur between the funded projects and other stakeholders, but such consultation was generally initiated by project staff during informal case management, rather than as part of a formal communication/outreach strategy.
6.5 In what way is service delivery similar or different among the models?
As noted previously, each of the five projects reviewed had considerable variation in program consultation, design, implementation and execution. While some projects (My Child, My Heart, ECIP) had a distinct dual focus in terms of supporting both the child and parents, other projects (Choose Life) seemed to be primarily focussed on providing services to children and youth.
Detailed in Table 2 is the program focus for the three case studies reviewed as part of this study.
| My Child/My Heart | Choose Life | Regina ECIP | |
|---|---|---|---|
| Enhanced case management | Yes | emerging | Yes |
| Introduction of new projects/activities | Yes | Yes | limited |
| Focus on parental supports | Yes | limited | Yes |
| Use of new staff/processes | Yes | Yes | Some new staff |
| Use of existing staff/support services | Yes | Yes Some new staff |
In terms of "functionality" of the projects, for the case studies conducted on projects that existed prior to receipt of Jordan's Principle funding, these projects tended to be able to roll-out services much more quickly than was the case for new projects. It was also observed that program management, case file administration and program activities varied on a site by site basis. This again reflects the fact that Health Canada did not prescribe (nor provide) program "tool kits" that would identify key program elements, reporting structures and/or consultation requirements. It should be noted however, that all programs collected some data and were interested to collecting the correct data to demonstrate outcomes, but were often unclear on what data was most appropriate.
6.6 What has changed under Jordan's Principle?
In discussions with program staff, stakeholders and parents, it appears that Jordan's Principle funding is generating a range of positive outcomes that are enhancing the health and quality of life for both youth and their parents.
Case study participants identified a range of outcomes associated with programs/services now available via Jordan's Principle. Among these include:
- Reduction in suicides/suicide attempts/other incidents;
- Improved cognitive and social functioning;
- Extension of services from children to youth;
- Improvement in school attendance and academic achievement;
- Increased ability for families to remain on‑reserve; and
- Improved environment for parents.
In addition to the impacts identified by program staff/stakeholders, parents who were interviewed as part of this Review were also very supportive of the program. Parents cited a number of benefits of the program (either via the funded project, or via direct application to Jordan's Principle to obtain financial support for services/other). The benefits/impacts identified by parents are summarized as follows:
- Active "champion" for family: Projects that included funding for enhanced case management (My Child, My Heart, ECIP Regina) generally included a "wrap around" case management approach in which the case managers would work with the child/family to obtain necessary support either under Jordan's Principle or from other community/social service agencies. This active support was seen as a very positive step in terms of assisting First Nation families navigating a complex service environment for children with various health conditions. Almost all parents talked about being better "able to parent" because of the supports provided by the case management worker as well as the Jordan's Principle funding for required supports/services. Parents were also very positive about the support they received from case managers who would identify what services/supports that they should apply for, assist such parents in applications, and generally serve as an advocate in their interactions with other education, health and social service agencies.
This program is a Godsend…we finally feel that we have someone on our side helping to make sure our daughter has access to the supports she needs..instead of fighting us, they are helping us.
The other major ways in which the Initiative had supported families included:
- Positive child outcomes from provided supports: Parents identified that receipt of funding for respite as well as other supports (i.e. adaptive technologies, home adaptation, other) were having a number of positive outcomes. Thus, parents for example noted that their child: could now attend school, could return to their care, communicate their needs, had a group of friends, were more readily accepted in the community, stayed in school, and demonstrated more positive coping mechanisms and behaviours. Parents also noted that the respite funding allowed them to find caregivers to take care of their children, many indicated that in the absence of such funding, they would have to consider temporarily "signing over" their children to a social service agency in order to get some relief from the 24/7 demands of their child with complex medical needs. Parents were also very positive in terms of other supports now available to them under Jordan's Principle, such as funding for child assessments, tutoring, learning technologies (iPads and learning/communication software) as well as funding for direct service provision (SLPs, OTs, other).
- Improved education outcomes: Parents and stakeholders interviewed as part of this research noted that the children who were now being supported via the Jordan's Principle funding were benefitting from such supports. Parents and stakeholders cited such improvements as increased school attendance, improved academic scores (due to tutoring and other supports) and access to additional educational supports given that some student assessments were "fast tracked" due to the ability of using Jordan's Principle funding to obtain such assessments.
It should be noted that it appears that Health Canada has yet to establish a reporting framework that moves beyond reporting on financial expenditures and activities (i.e. numbers of children served). While the research team was not supplied with the annual reports submitted by the projects to Health Canada, it was noted that such reports did not ask the project proponents to identify the "impacts" or outcomes associated with such funding. While stakeholders were in agreement that their projects were having a positive impact, they noted that they did not currently track such outcomes as this information was not requested by Health Canada or they were uncertain about what should be tracked and how.
6.7 To what extent has Jordan's Principle contributed to the creation/improvement of partnerships, processes and service coordination through these initiatives?
Stakeholders noted that as part of their program roll-out, they would undertake consultations with communities and service providers as to program objectives and elements. As noted previously, it does not appear that programs were designed in a stepwise manner (i.e. where one would expect to see funding for program coordination and consultation, funding for program design, and funding for program implementation). Coordination of services was likely improved under Jordan's Principle, but for the projects that were visited, the research team could not observe a high degree of service coordination (although relationships certainly exist with referral agencies). Programs were all aware of the concept of case management, but were in different stages of implementing case management approaches for the children and youth they serviced. As the case management approaches were formalized, programs expected that greater service coordination would occur. Programs with the greatest service coordination had existing service partnerships or relationships in place prior to the initiative funding.
As noted previously, while it appears that service coordination likely improved, it is likely due to the work done at the staff level (i.e. case managers consulting with other service providers), rather than at the program level. The Research Team did not see evidence of formal structures that would indicate a high degree of service coordination (re: no community service asset map, no inter-agency Memoranda of Understanding, other) although given the few sites visited, this may not be indicative of all projects/programs funded under Jordan's Principle.
7. What are the Key Strengths and Challenges, and what are the Lessons Learned?
7.1 Key Strengths and Challenges
As noted throughout this report, Jordan's Principle funding has resulted in a number of positive outcomes and reflects a new process in which programs/services can be provided to First Nation youth (and their families) with complex medical conditions. However, the very rapid roll-out of the program, with very limited support resulted in considerable challenges for projects that were "new" and did not benefit from pre-existing structures, staff and/or relationships with other service partners. Based on the three case studies completed, the strength and challenges of Jordan's Principle funding is summarized in Table 3.
| Strengths | Challenges |
|---|---|
|
|
|
|
|
|
|
|
|
|
7.2 Lessons Learned
Highlighted are the key lessons learned from the Review of Jordan's Principle. As noted earlier, given the very limited lines of evidence used in this Review, these "lessons learned" must be interpreted with caution.
Project or program effectiveness varies considerably on the basis of prior program history
The results of the Review suggest that program implementation (and ultimately program effectiveness) is highly correlated with the prior history of the project or program. For example, from the case studies, programs that were in operation prior to Jordan's Principle funding (My Child, My Heart, ECIPs) were much better able to launch "new" programs/services as they had existing program administration, management structures and relationships in place. In contrast, projects that were only just started as a result of Jordan's Principle (Choose Life) experienced significant challenges in terms of program design, implementation and service delivery.
Need for clear program theory underpinning programming actives
As noted previously, some programs were unclear if the activities they were completing clearly linked to the outcomes they were seeking (i.e. positive mental health outcomes). Good program design requires sound theories of change that show the link between program activities and the desired program outcomes. Simply developing a robust program theory and implementing it could take two years. At the community level, communities did not have the capacity to complete such a task, and as noted, nor did the administrative organization. Time is required for the administrative organization to build this capacity prior to rolling out program funding. Thus program design funding is required prior to program funding.
It should be noted however, that given the CHRT's ruling that applications be reviewed within a 12 to 48 hour timeline, the challenges associated with program design/implementation reflect a desire to satisfy CHRT's vision of "quick" service delivery to meet unmet needs, as opposed to a more comprehensive approach that would likely have better addressed program design and implementation issues.
More guidance /support should be provided to newly developed programs funded under Jordan's Principle
It is clear that given the limited funding window, projects and programs were often "rushed" in order to meet financial targets. However, such an approach resulted in disjointed service delivery and ultimately, development of programs in isolation of broader community requirements. In the future, "new" project or programs funded under Jordan's Principle should be funded in a staged approach. These stages could include:
Figure 1
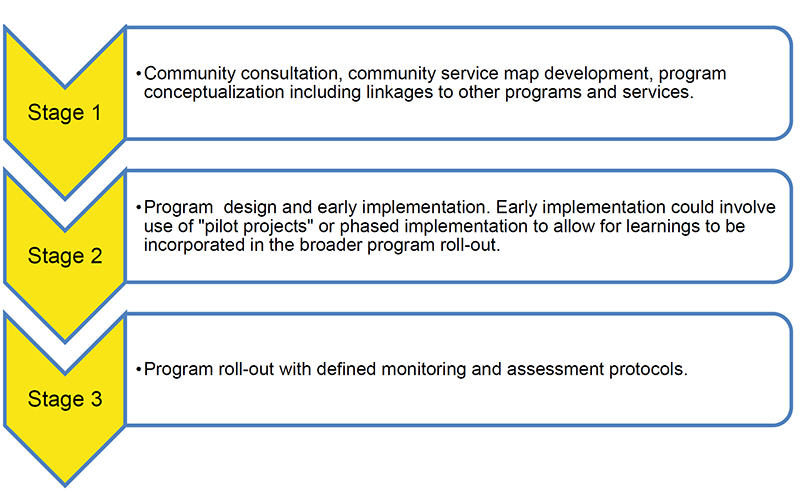
Text alternative for Figure 1
The figure depicts the three stages of Program Delivery.
The first, Stage 1, is described as "Community consultation, community service map development, program conceptualization including linkages to other programs and services."
The second, Stage 2, is described as "Program design and early implementation. Early implementation could involve use of "pilot projects" or phased implementation to allow for learnings to be incorporated in the broader program roll-out."
The final, Stage 3, is described as "Program roll-out with defined monitoring and assessment protocols."
Examples of supports that could have been developed by the administrative organization and made available at the community level would include:
- Workshops outlining Jordan's Principle;
- Workshops on application completion;
- Workshops and toolkits on program design;
- Workshops and toolkits on theories of change, logic models and program monitoring and measurement;
- Toolkits with commonly used program protocols such as intake forms and consent forms; and
- Workshops on Human Resources processes for hiring, contract development, etc.
Address Capacity and Infrastructure Challenges
Under Jordan's Principle funding, there was a desire to implement new programs and services, many of which required trained and qualified health professionals, as well as the need to hire significant numbers of staff to work in the programs/projects. It was clear that while Jordan's Principle resulted in the injection of considerable resources to meet community need, there were gaps/challenges in terms of having the available infrastructure (offices, space, other) and human resources (trained and qualified health staff, project coordinators, various support workers etc.) to effectively support the funded programs/projects. In this context, it would be important to not only provide funding to support programs, but a portion of the funding under Jordan's Principle could be earmarked for infrastructure and/or other capacity building at the community level.
Appendix A: My Child, My Heart Case Report
Niniijaanis Nide – My Child, My Heart Program
Program Review – Community Visit Summary
1. Community Background
Pinaymootang First Nation is part of Manitoba's Interlake Region, within Treaty 2 territory. The community is situated approximately 250 km north of Winnipeg along Highway 6 on Fairford 50 Reserve. The band has approximately 3,258 members: 1,271 living on‑reserve and 1,987 residing elsewhere.Footnote 6 As compared to the rest of Canada, the population of Pinaymootang First Nation is young, with 50 percent of its members under the age of 20.Footnote 7
Pinaymootang First Nation is a member of the Interlake Reserves Tribal Council Incorporated. Chief Garnet Woodhouse and Council were elected in October of 2017. The Nation began receiving Block Funding in 1998.
The community has a wide range of services, including a school, administration office, daycare, fire/police protection services, water plant, three community churches, employment and training facility, Child and Family Services, sewage/garbage disposal, postal services and health services.
The Pinaymootang First Nation Health Centre provides health services with the aim of promoting healthy lifestyles and improving access to reduce health inequalities. The Niniijaanis Nide: My Child, My Heart Program, currently funded through Jordan's Principle, is housed within the Health Centre. The Health Centre employs 26 staff. The expanded Health Centre opened on July 4, 2018, and includes additional examination rooms, office spaces, as well as a kitchen and meeting/event room.
2. My Child, My Heart Program Overview
2.1 Program History
As a pilot program, My Child, My Heart (Integrated Approach to Services for Families with Children with Complex Needs) began operating in 2015, under Health Services Integration Funding, through collaboration between Pinaymootang Health Centre, Anishinaabe Child and Family Services, Pinaymootang School, Pinaymootang Social Program and Health Canada, First Nations Inuit Health Branch (Manitoba Region). The pilot ran from December 15, 2015, to March 31, 2017, under Health Services Integration Funding.
The pilot resulted from a complaint filed by a Pinaymootang family with the Canadian Human Rights Commission, which argued that their child's complex health care needs were not met by the services available in the community. Health Canada's subsequent request to the Pinaymootang Health Centre to submit a proposal to meet the needs of this child lead the centre to instead submit a proposal to meet the needs of 11 families of children with special health care needs thus fulfilling their role as health care advocate for the community.
From April 2017 to March 31, 2018, as well as in the current fiscal year (April 2018 to March 2019), My Child, My Heart was funded through Jordan's Principle.
2.2 Program Objectives
The goal of Niijaanis Nide: My Child, My Heart is to allow children to access services where their families and support networks are located and in a home setting where they feel comfortable and safe. My Child, My Heart has six key values: Footnote 8
- Children are best cared for at home and within families;
- Special needs of children and families have to be met as well as their basic needs;
- Parents know their child better than anyone else and must be treated respectfully;
- Professional supports must be coordinated and responsive to the needs of individual children and families;
- Identify risks to be managed in ways that provide safety and good quality of life to the child and family; and
- Partnership working across disciplines and agencies is essential.
My Child, My Heart supports children with complex needs in Pinaymootang from birth to 21 years of age. Children can live on- or off‑reserve. Children with complex health care needs are defined as children with a congenital or acquired long-term condition that are attributed to impairment of the brain and/or neuromuscular system that create functional limitations.
3. My Child, My Heart Program Operations
A Community Advisory Committee provides oversight to the program, with members representing health, education, and social programming.
3.1 Staff
The program includes:
- One Case Manager/Project Coordinator;
- One full-time equivalent (FTE) Nurse or Social Worker;
- Three to five FTE's Child Development Worker (CDW), Health Care Aids or Early Childhood Educators (ECE's);
- Ten part-time respite workers for evening and weekend family respite; and
- One Administrative Assistant/data entry position.
3.2 Services
A wide range of activities are carried out by the program:
- Provide evening and weekend respite care for families;
- Collaborate with service providers;
- Advocate for continuum of care for children with complex needs;
- Provide a continuum of family training;
- Build partnerships across disciplines and agencies within the community that provide services to the children with complex needs;
- Provide staff education and training related to caring for children with complex needs;
- Provide day and evening programming for children with complex needs; and
- Provide one-on-one work between the CDW and the child.
Many of the services are provided in the Pinaymootang First Nation Health Centre. The addition of the kitchen and meeting room in July 2018 has enabled the program to hold day and evening programs for children and families.
The program has developed a program delivery process aimed at providing continuous, integrated care to children with complex needs so as to allow them to remain living in Pinaymootang. The five phase program delivery process is as followsFootnote 9:
- Phase 1: Establishing a relationship:
- Meet with the child and parent to allow them to share the child's strengths, challenges and preferences. The phase allows workers to get to know the family and child and establish trust.
- Phase 2: Identifying needs and objectives:
- Identify what the parents want for their child.
- Develop one to three objectives with the CDW.
- For each objective, develop benchmarks for goal attainment and scales to measure attainment of goals.
- Phase 3: Implementing the program:
- The CDW implements the program based on the goals and objectives identified in Phase 2.
- There are two components to program implementation:
- Basic Care and Support (e.g. occupational therapy (OT) and physical therapy (PT)); and
- Goal-Oriented Work (e.g. behavioural goals).
- Phase 4: Generalizing Goals:
- The CDW works with the child, family and others to ensure objectives are generalized across different people and different settings using a variety of materials and tools.
- The CDW support and coach the parents/caregivers and train any secondary caregiver.
- Services are provided in different environments (home or school) using a variety of resources.
- Phase 5: Conducting evaluation and providing continuing care support needs:
- Provide support to parents and caregivers and evaluate continuing basic care and support needs.
- The following are evaluated:
- Child-oriented goals; and
- Family-oriented goals; (stress and coping mechanisms);
3.3 Case Management
Once a child's service plan is developed the program holds regular case management meetings with the necessary service providers to discuss implementation, provision and generalization of services for each child. The families are included in the case management meetings. Case management is critical to continuity of care and ensures that teaching and services are reinforced and provided across a wide range of environments including the home, school and community. All service providers interviewed stressed the importance of the case management meetings and noted that the program has successfully leveraged the case management model in part due to the strong partnerships that the program has established.
3.4 Partnerships and Service Providers
The program has established a number of partnerships or working relationships which allow the provision of services to children with complex needs within the community. While in the pilot phase My Child, My Heart began working with several partners to provide services to the 11 families. The range of partnerships has since expanded with the introduction of funding through Jordan's Principle. In the case of the Rehabilitation Centre for Children, the St. Amant Centre, and the Manitoba Adolescent Treatment Centre, the services partners, at the request of ISC (formally (INAC), have established contractual preferred service provider relationships that allows provision of services to children with complex needs on any reserve across Manitoba. These contracts were developed through a proposal-based procurement process and are funded by Jordan's Principle.
Pinaymootang First Nation Health Centre: the centre provides significant in-kind contributions to the program, including office space for their staff, program space and program oversight (the salary of the Health Director is entirely covered by other funding although they are involved in program oversight). Additionally, the centre is accredited which helps to ensure the overall quality of all services provided to children with complex health care needs within the centre.
Pinaymootang School: representatives of the school sit on the Community Advisory Committee and attend the case management meetings as needed. The school works with the program to coordinate services provided to children in school by Special Educational Assistants and CDWs. Support to children with complex needs while in school is funded through the school budget. Since the implementation of the program, the school has noted improved attendance among children with complex health needs, as well as improved integration and inclusion by other children. School representatives were unable to speak to improved academic performance. The school is currently not concerned about being able to meet the needs of children with complex health care needs during school hours.
Pinaymootang Daycare: the program works with the staff of the daycare to identify children potentially in need of services. The daycare refers families to the program if it is believed that special services may be required.
Anishinaabe Child and Family Services: coordinates services provided through the agency and My Child, My Heart, including in-home care services, during case management meetings.
Rehabilitation Centre for Children: provides OT, PT and speech therapy to children in the program. Given the Centres' more recent involvement in the program roles, responsibilities and communication lines are still being established between the Rehabilitation Centre for Children, the program and other service providers. High levels of investment from My Child, My Heart case managers have supported the introduction of services from the Rehabilitation Centre for Children to date. As well as providing OT, PT and speech therapy to children in the program, the Rehabilitation Centre for Children has completed training with program staff, and provided developmental checklists to community service providers to assist them in identifying children that should be referred to the My Child, My Heart program. Additionally, the Rehabilitation Centre for Children has developed and provided to the program a brochure explaining the services they provide for distribution among families. Representatives from the Rehabilitation Centre for Children noted that the program had resulted in developmental delays among community children being caught and treated earlier. Further, interviewees noted that necessary equipment that was not covered through Non-Insured Health Benefits has been provided through My Child, My Heart program funding.
St. Amant Centre: a basket of services are available to the My Child, My Heart program children and families through the St. Amant Centre including: non-crisis counselling for parents, siblings and the child, the family care program (advocacy and navigation), dietician services (dealing with challenging eating), and counselling for dealing with challenging behaviour in children with complex health care needs. Uptake of the St. Amant Centre services has been high among program families. As with other newer service providers, the St. Amant Centre works directly with the program case management team to coordinate and deliver services. The centre has also provided training to school staff to better support the children in the program. The centre noted improved family dynamics in the home, reduced difficult behaviours among the children, and increased positive behaviours in children (e.g. using the toilet, traveling in a vehicle, and return to school). The center is still working to establish an appropriate caseload for their staff but have needed to hire additional staff to meet demand for services from this program and other programs across Manitoba. A significant outcome noted by interviewees from the centre was the reunification of one child with their family and the planned reunification of another. In both cases, the children could now return to Pinaymootang where services are available rather than staying in a special care facility to have their needs met. Interviewees also noted that parents previously considering putting their child in a full-time care facility were no longer considering this option.
Manitoba Adolescent Treatment Centre: has worked with the My Child, My Heart program for four years providing mental health and psychiatric services, including preliminary assessments, arranging initial consultations for diagnosis, and ensuring medication is obtained. The centre provides mental health supports to youth, their families, and will consult with other service providers and the school. Consultations with psychiatrists and counsellors are completed through Tele-Health at the Pinaymootang First Nation Health Centre; in-person consultations can be scheduled if the doctor feels it is needed. After diagnosis, ongoing monitoring and prescription renewal is completed by community-based physicians that visit the Pinaymootang First Nation Health Centre. Barriers to service access noted by the interviewee included access to Manitoba Tele-Health, which is in high demand. Additionally, the central location of the Tele-Health equipment reduces privacy and can introduce confidentiality concerns. Clinicians stay in direct contact with the child's CDW to support case management as required. The Manitoba Adolescent Treatment Centre is still working with the service providers within My Child, My Heart to define roles, responsibilities and lines of communication on a case-by-case basis. Regular meetings among service provider management were said to be helping to support collaboration and the establishment of clear roles and responsibilities. The most significant challenges noted by the interviewee to the provision of services is the availability of on-the-ground support for individuals who are a threat to themselves or others. While this was not noted as a concern in the My Child, My Heart program, it has been noted in more remote programs in isolated communities.
Eagle Urban Treatment Centre: the My Child, My Heart program provides families referrals to the Eagle Urban Treatment Centre when they are leaving Pinaymootang to relocate elsewhere in Manitoba. Conversely, the centre notifies the program when a family is returning to the community to ensure continuity of services. Within Manitoba communities, the Eagle Urban Treatment Centre provides advocacy and referral to families. Advocacy was said to be important to support families navigating the provincial system to ensure children with complex health needs receive the required services under Jordan's Principle.
3.5 Program Outreach
The program received referrals from service providers as well as services in the community (school, daycare, etc.). Additionally, the program advertised available services through various methods including booths during community events.
3.6 Scope of Service Provision
Currently, My Child, My Heart provides services to approximately 60 children, many of whom receive ongoing support. Of the 60 children, 15 are currently transitioning to school, 12 received support services and 33 are actively involved in the program. Examples of the types of services provided included:
- Day program activities (reading club, physical activity night, "nagamon" music club, Moe the Mouse-read);
- Parent support meetings;
- Parent and caregiver classes;
- American Sign Language training for two families;
- Physiotherapy and occupational therapy;
- Speech and language therapy and audiology therapy;
- Visual therapy;
- Dietician services;
- Behavioural/cognitive behavioural therapy;
- Psychologist and psychiatrist consultations, spiritual wellness supports, and mental health therapy;
- Child development supports (individual);
- Home modifications;
- Home visits for extended families; and
- Respite care.
3.7 Program Budget
The annual budget for the My Child, My Heart program during the years it was funded through Jordan's Principle is shown in the Table 4. Across both years, the budget has remained the same, with it costing approximately $12,660 per child (60 children) to provide service. In addition to the core budget, the program received one-time funding for a handibus ($78,864.32) and American Sign Language Training (training: $7,800 plus facilitator travel: $1,560). In should be noted that the Pinaymootang First Nation Health Centre provides in-kind resources (facility space and utilities), which would need to be covered under the project budget if this facility was not available.
| Program Expenses | Annual Budget | |
|---|---|---|
| 2017-18 | 2018-19 | |
| Case Manager/Project Coordinator (One FTE Nurse or Social Worker) | $75,000 | $75,000 |
| CDW, Health Care Aids, or ECE's (Three FTEs; $39,000 each) | $117,000 | $117,000 |
| Ten part-time respite workers for evening and weekend family respite ($27,000 each) | $270,000 | $270,000 |
| Administrative Assistant/data entry position | $35,000 | $35,000 |
| Employee Benefits (14 percent) | $69,580 | $69,580 |
| Total Staff | $566,580 | $566,580 |
| Staff Training/Professional Development | $36,000 | $36,000 |
| Travel | $28,000 | $28,000 |
| Program Activities | $60,000 | $60,000 |
| Sub Total | $690,580 | $690,580 |
| Admin Fee's (10 percent) | $69,058 | $69,058 |
| Grand Total | $759,638 | $759,638 |
3.8 Monitoring of Child and Family Outcomes
The program monitors child and family outcomes at three, six, nine and 12-months post-intake. A goal attainment scale is used to determine if the family has been able to meet the goals they set for their child. Standardized tests used by the program include the:
- Measure of Processes of Care (20-item measure on parents' perception and satisfaction of the services provided for their child);
- Parenting Stress Index – Short Form (36-item measure tool that documents levels of stress – whether or not families are feeling supported);
- Social Support Index (17-item measure that taps into parents' experience of their support networks both with and outside the family); and
- Family Quality of Life (25-item measure that evaluates family quality of life, through five domains):
- Family Interaction;
- Parenting;
- Emotional Well-Being;
- Physical/Mental Well Being and;
- Disability Related Supports.
3.9 Program Outcomes
In 2016, the Canadian Home Care Association published a report on the impacts of the My Child, My Heart program. Among children, increased independence, socialization and sense of accomplishment were all observed. This was accompanied by a decrease in problematic behaviours. As a result of their interaction with the program, parents and caregivers were said to have increased connection with their child, trust in the health system, feelings of competency, coping, connection with other parents and ability to actively participate in the child's care.
Service providers were unanimous in their agreement that without My Child, My Heart, children with complex health needs living on Pinaymootang First Nation Reserve would be unable to access the necessary services required to meet their needs. Without such services these children were less likely to attend school, remained socially-isolated, and were unable to reach their potential. Further, many families would be unable to remain in the community if these supports were not available.
Parents who attended the focus group all felt that they had received the supports they required for their children through the program. Parents were unable to list gaps in supports and felt that the available services were meeting their child's immediate and long-term needs. Parents noted that their children's behaviour was more manageable and their children were less socially-isolated. Respite care was appreciated, as was the ability to share stories with other parents. Parents noted that they felt less isolated and that the program had helped take away feelings of self‑doubt or blame that their child's development or behavioural challenges were their fault. Some of the children had returned to school or began attending school for the first time as a result of the support. Many parents stressed that without the program they would need to move to Winnipeg to ensure their child's needs were met; however, in doing so, they would be left without social, emotional and respite support from friends and family.
3.10 Program Challenges
Given the length of time the program had been operating and strong program leadership, the My Child, My Heart program was experiencing few challenges. Program staff, however, estimated that they had been unable to reach all children with complex health needs who required support within the community; in part due to the reluctance of parents to have their children assessed. Program leaders also acknowledged that many families with high needs children had relocated to urban centres to assess provincial supports and had not yet decided to return to the community now that on-reserve supports had increased. It was expected that demand for services would increase as families displaced during the 2011 flood began moving home. The expansion of the Pinaymootang First Nation Health Centre had resolved the program's facility challenges, as there was now sufficient space for program staff and programming activities. Staffing was also not a challenge for the program as individuals with the necessary skills reside in the community.
The most significant challenges highlighted by stakeholders interviewed were:
- Uncertainty of funding; and
- Lack of funding for individuals aged 22 and older.
Without long-term funding, the program is less able to plan and retain staff. The uncertainty of funding also impacts families who were unclear what they would do if funding was discontinued.
Lack of funding for individuals with complex health needs aged 22 years and older was universally seen as the biggest program challenge. Stakeholders noted that the need for support services on‑reserve for adults (aged 22 and older) remains unmet. Currently, when youth "age-out" of program, the only source of funding to meet their needs is Home Care.
In January of 2016, the Pinaymootang First Nation Health Centre submitted a proposal to INAC to provide young people with complex needs with the support required to transition into adulthood; the proposal was not accepted.
4. My Child, My Heart Program Special Projects
In 2017, My Child, My Heart applied for one-time project funding to develop practice standards and guidelines for implementing Jordan's Principle in First Nation communities across Manitoba. The goals of the project were toFootnote 10:
- Lead the development of Practice Standards and Program Guidelines to support regional implementation of Jordan's Principle across Manitoba;
- Coordinate regional engagement to ensure First Nations lead the development and implementation of Jordan's Principle in every First Nation community; and
- Coordinate stakeholder engagement to ensure input from key stakeholders and service providers into the design of core program components, standards and tools for community-based service delivery as well as regional service coordination.
The Community Advisory Committee developed a Jordan's Principle Regional Working Group to support the achievement of the three coordination goals (previously listed). The budget for this project was $265,852.76. The process utilized to develop the practice standards and guidelines was as followsFootnote 11:
- Project Planning: lead by the Pinaymootang Health Centre Director and Case Manager for the Niniijaanis Nide Program.
- Reviewed the Niniijaanis Nide Program to determine what process and policy could be built on;
- Coordinated and facilitated two planning meetings; and
- Identified themes essential to the guidelines and standards:
- Referral Map Process – including referrals to different aspects of services,
- Utilization of Tele-health capabilities,
- Review Independent Education Plan and behaviour Intervention Plan templates to ensure they align with Jordan's Principle Standards,
- Parental consent throughout all processes,
- Communication mechanisms and standards,
- Visual Services Chart, and
- Literature review of other regions for practice standards for Jordan's Principle.
- Draft Program Standards and Guidelines.
- Engagement Workshops: four held with First Nations and government representatives in four areas including Social Development, Family Supports and Services, Health and Education – refining the standards and guidelines with each session.
- Finalize the Program Standards and Guidelines as a Toolkit with five modules (Creating Community Teams and inter-Agency Collaboration, Community Program Development, Work Plan Development, Program Evaluation and Monitoring, and Data Collection).
As a result of this project work, the My Child, My Heart program was able to:
- Develop an Implementation Toolkit for Jordan's Principle Practice Standards and Program Guidelines; and
- Present the Toolkit to teams from 63 First Nations in Winnipeg on March 29-31, 2017.
The staff of the My Child, My Heart program continue to support other First Nation communities through informal meetings to understand how to implement and maintain a program under Jordan's Principle. This work is done in addition to their core work responsibilities.
5. Lessons Learned
When considering how to implement similar programming in other First Nation on-reserve communities across Canada, significant lessons can be gained from the successes of My Child, My Heart. The program's early experience as a pilot meant they were operationally ready to expand programming when funding under Jordan's Principle became available. Further, their work in developing practice standards and guidelines for implementing Jordan's Principle in First Nation communities helped to provided best practices for program implementation.
The review (document review, site visit and key informant interviews) highlighted several key factors, which contributed to the program's past and continued success. These factors are:
Community Governance Structure: The governance structure of Pinaymootang First Nation positively supported the My Child, My Heart program in a number of ways. The program had strong support from Chief and Council, who took the approach of "hiring the correct staff" and letting them run the program based on their knowledge and experience. Further, Pinaymootang First Nation received Block Funding, which meant that the Pinaymootang First Nation Health Centre could apply for accreditation, which they ultimately did receive. Key informants noted that facility accreditation helped to ensure the facility was run optimally to best meet community need. Accreditation may also be correlated with the provision of a wider range of services and greater service integration.
Community Consultation: My Child, My Heart began operating in response to direct community needs. The initial funding proposal was created to meet the specific needs of 11 Pinaymootang First Nation families. Further, community needs and barriers to service were also outlined in the report developed in conjunction with McGill University.Footnote 12 Key informants attributed also the success of the My Child, My Heart program to the fact that they had listened and responded to the needs of the community.
Interagency Collaboration: All key informants stressed that interagency collaboration was critical in a project of this nature. Service provision must be managed across multiple settings (e.g. home and school) and agencies that have established working relationships are better able to collaborate and develop clear roles and responsibilities. Since My Child, My Heart began operating in 2014, they had three years to establish relationships with community organizations and service providers before their client load expanded. Additionally, the Health Director's experience in ensuring that the Health Centre worked "separately but together" with other community services greatly benefited the program.
Multidisciplinary Teams and Case Management: To provide holistic child centered care, key informants noted that multidisciplinary teams that effectively use case management must be in place. My Child, My Heart's "Circle of Care" model emphasizes a comprehensive and holistic approach to care, which looks at the child from the prospective of physical, cognitive, social/emotional, spiritual and communication development, as well as acknowledging the need for a health-supported family unit. As a best practice, My Child, My Heart held regular case management meetings with families, CDW and relevant service providers to ensure the family and child goals were being met. Additionally, a wide range of practitioners were available to consult with the child and meet their unique needs.
Strong Leadership:One key informant noted that program managers operating a program such as My Child, My Heart must possess a unique set of skills in ensuring project success. Specifically, an individual running such a program must understand the community and its members' needs; the individual must also act as a "community champion" who is able to run the program while simultaneously building capacity.
Infrastructure: Pinaymootang First Nation had basic infrastructure in place to support programming at all levels, including the newly-expanded Pinaymootang First Nation Health Centre, which provides in-kind contributions to the program. A community attempting to develop and implement a program under Jordan's Principle would be disadvantaged without existing infrastructure.
Capacity Building and Education: Staff of My Child, My Heart believed that they had not yet reached all of the children in need within the community, in part because some parents were still reluctant to have their children assessed. Further, one key informant observed that many community members did not see the need for special needs programming since they falsely believed that children with complex health care needs did not live in the community. Staff felt that educating parents was part of the program's role, as was removing the stigma associated with providing children with complex health needs and their families' specialized supports. Many of the service providers interviewed had an educational component associated with the services they provided.
Access to Service: My Child, My Heart had been operating two years prior to Jordan's Principle funding. During this time the program worked to establish relationships with services providers. The community, while remote, is still accessible by car and many health care professionals provided services at the health centre. A more remote community, however, would have been challenged to access appropriate services providers. The third party service agreements currently in place with such organization as Rehabilitation Centre for Children, St. Amant Centre, and Eagle Urban Treatment Centre could assist smaller and more remote communities' access appropriate services.
Appendix B: Choose Life Case Report
NISHNAWBE ASKI NATION – CHOOSE LIFE
September 19-20, 2018
1. Background
Choose Life is funded under Jordan's Principle and run through the Nishnawbe Aski Nation. NAN, a political territorial organization, previously known as the Grand Council Treaty Nine until 1983, consists of 49 communities in northern Ontario.Footnote 13 Of these communities, 43 are affiliated with seven tribal councils, including: Windigo First Nations Council, Wabun Tribal Council, Shibogama First Nations Council, Mushkegowuk Council, Matawa First Nations, Keewaytinook Okimakanak, and Independent First Nations Alliance while the remaining six communities do not have a tribal council affiliation.Footnote 14 NAN includes the James Bay Treaty Nine and also a segment of Treaty Five (in Ontario) extending over 210,000 square miles.Footnote 15 To put this into perspective, NAN covers two‑thirds of Ontario's land mass.Footnote 16 NAN has four major traditional languages including OjiCree (West), Ojibway (Central – South), Cree and Algonquin.Footnote 17 Across the 49 communities, both on- and off-reserve members are estimated to account for approximately 45,000 people.Footnote 18
Figure 2 illustrates the NAN territory, including member communities, their nearest emergency care services and road access.Footnote 19 The majority of NAN communities are highly isolated, specifically:
- A majority of NAN First Nation communities do not have full access to permanent roads but rather have seasonal accessibility, with approximately half of the NAN community members living in communities without permanent road access;
- There is very little access to Level I / Level II trauma centres: for many, emergency department care is accessible only by plane or helicopter;
- There is very little access to northern referral centres; and
- There are First Nation community hospitals but they are not accessible to many NAN communities.
Figure 2: Nishnawbe Aski Nation Member Communities Map
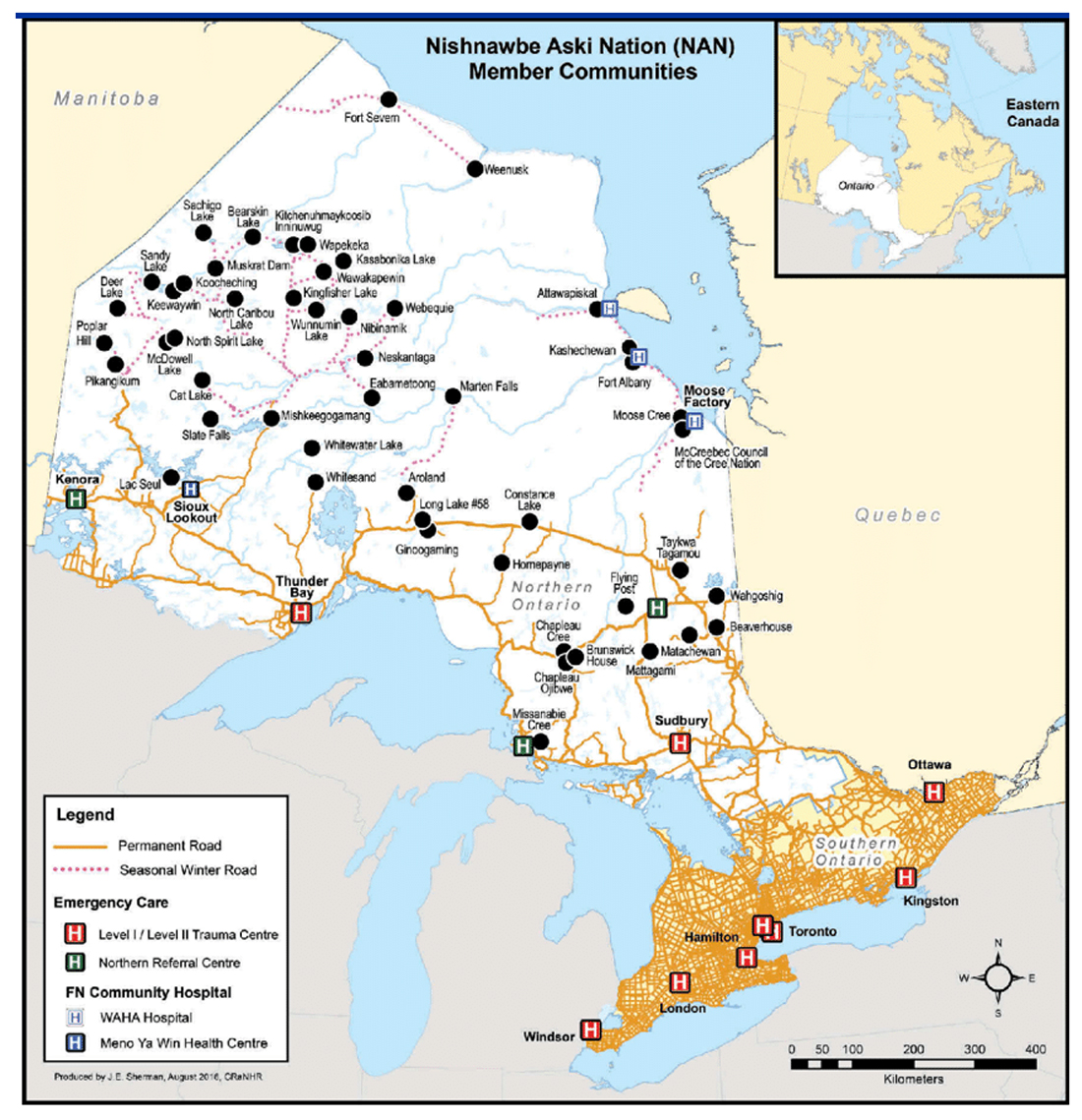
Text alternative for Figure 2: Nishnawbe Aski Nation Member Communities Map
Figure 2 is a map of Ontario identifying the 49 Nishnawbe Aski Nation Member Communities. The map identifies roadways (permanent road systems and seasonal winter roads), Emergency Care Facilities (Level I/Level II Trauma Centres and Northern Referral Centres), and First Nation Community Hospitals (WAHA Hospitals and the Meno Ya Win Health Centre). There is also a smaller detail map of the Eastern part of Canada, situating Ontario’s location within this part of the country.
NAN follows a self-determination model, which includes acquiring a spiritual, cultural, social and economic independence as a sovereign nationhood. The specific objectives of NAN includeFootnote 20:
- "Implementing advocacy and policy directives from NAN Chiefs-in-Assembly;
- Advocating to improve the quality of life for the people in areas of education, lands and resources, health, governance, and justice;
- Improving the awareness and sustainability of traditions, culture, and language of the people through unity and nationhood;
- Developing and implementing policies, which reflect the aspirations and betterment of the people; and
- Developing strong partnerships with other organizations."
NAN acts as an advocate for the communities that it serves, as such it has taken on the role of coordinating funding applications for Choose Life programs submitted by NAN communities.
2. Method
Choose Life operates in 47 of NAN's 49 communities. As of July 31, 2018, the NAN Choose Life program had funded 122 projects in the NAN territory.Footnote 21 A significant proportion of funding was given for land-based mental health services (32 million).Footnote 22
- To select the one to two projects that would be visited as part of the review, Malatest contacted NAN's Choose Life Coordinator and Choose Life administrative staff who suggested two programs; one run by Keewaytinook Okimakanak Secondary School Services and the other by Lac Seul First Nation. Both programs included a land-based program component. The program run through KOSSS had been operating for approximately a year and half, while Lac Seul First Nation's program had only been in operation for five months.
- It is important to note that given funding and time constraints, this review was only able to speak with staff from two of the 122 funded Choose Life programs. As well, neither program was located in any of the extremely remote communities represented by NAN. Findings therefore represent a preliminary snap shot of Choose Life programming and thus cannot speak to the effectiveness or efficiency of the Choose Life program overall.
As part of the review, the researchers conducted the following interviews with the KOSSS and Lac Seul Programs:
- Interview with KOSSS Choose Life program coordinator;
- Interviews with KOSSS Well Being Workers (n=4)
- Interview with KOSSS Intervention Site Coordinator
- Interviews with KOSSS Student Support Worker
- Interview with KOSSS Social Counselor
- Interview with parent of student enrolled in KOSSS Choose Life
- Group interview with Lac Seul program staff (Program Coordinator, Land Based Coordinator and Land Based Workers (2), Community Chief, and Program Administrator)
3. Choose Life Program Overview
3.1 Program History
As a two-year pilot program, Choose Life began operating in 2017 under Jordan's Principle with the 49 NAN communities.Footnote 23 The program will operate until fiscal year 2018‑19 year under current funding. Choose Life was established as a requested order to the Canadian Human Rights Tribunal on behalf of NAN as there was acknowledgement that northern First Nation communities were being systemically discriminated against with regards to the provision of services and funding for mental health in the area.
3.2 Program Objectives
Choose Life is designed to:
- Fast track proposals for youth mental health prevention program/services regardless of the timing of their submission;
- Allow the development of appropriate services for NAN youth;
- Enhance mental health services for youth; and
- Incorporate healing activities that focus on culture (holistic approaches such as land-based programming).
4. Choose Life Program Operations
4.1 Scope of Services
In the fiscal year 2017‑2018 year, FNIHB, ISC provided 27,445,716 in funding for 57 applications, which equated to 12,222 youth receiving support.Footnote 24 Funding of 62,247,736 for 64 applications has already been provided in the fiscal 2018‑2019 year. This equates to 20,170 youth receiving support.
4.2 Application Criteria
In order to be considered, a NAN Choose Life application must meet the following criteria:
- Be submitted by a First Nation community located in the NAN territory;
- Include programming that targets youth at a serious risk of suicide; and
- Include a service delivery plan, which includes land based activities or a land based prevention and intervention program.
4.3 Application Process
The process of applying and successfully being granted program funding includes:Footnote 25
- Plan tasks and expected outcomes: a program plan must be put forward that outlines the expected outcomes of the program activities;
- Rationale: the program plan must give a rational as to why the services are needed in the community (e.g. community profile of youth; current mental health status of youth; evidence of suicide/suicide attempts/suicide risks);
- Tasks outline: the program must outline what tasks will be completed and by whom (e.g. who/what/approach and philosophy/required training/accountability);
- Budget outline and analysis: the program budget should be outlined and include descriptions of costs such as salaries/benefits, rent, training, travel, land based activities, materials, and computers;
- NAN application review: NAN reviews the community application looking at such things as the community, number of children served, program dates and budget request;
- ISC review and approval process: ISC reviews the application and provides immediate crisis intervention supports if necessary during the application process;
- Appeals process: should an application be declined by ISC, the Choose Life Working Group will discuss and review the application (No applications have been denied as of July 31st, 2018);
- Interim reporting: programs must report 45 days following the last day of September. Reports must indicate the number of children that have received services as well as a comprehensive cost total by services/support;
- Programming reporting: programs must provide an annual report by July 29th of the applicable fiscal year. This report must specify the services provided and the number of children receiving these services and supports, total cost, challenges and future needs;
- Financial reporting: there are annual audits and a ISC Internal Tracking Sheet for financial reporting; and
- NAN Choose Life revised budget submission: at times, a program may require additional funding. Choose Life has a format for the revised budget submission.
4.4 Challenges Associated with Program Design
Due to the short program implementation time frame, NAN was required to be "up and running" immediately. Issues associated with the short implementation window included:
- Insufficient training for the NAN Choose Life Staff: staff did not receive training in application/proposal development or application review.
- Insufficient NAN staff to provide adequate supports to the NAN communities: Initially, Choose Life was rolled out by NAN with only one staff person. An additional person was later hired, however, more staff and training would be needed if NAN was to be able to provide further administrative or program supports to the 122 programs funded under Choose Life.
- Poor direction from INAC on program reporting requirements: NAN staff noted that they required a better understanding of INAC's (ISC) reporting requirements so that they could better guide communities in completing the interim and annual reports.
- Lack of time for community collaboration: The short funding timeframe meant that communities did not have time to collaborate or learn from one another during the application process or program implementation phase.
- Insufficient communication to the communities from INAC: NAN staff noted that it would have been more effective if INAC had initially made community health directors aware of the Choose Life program.
Since NAN staff were involved in the development of community applications, they were familiar with the challenges communities commonly experienced when developing their Choose Life applications. Thus communities commonly lack:
- Safe and private spaces for programming (e.g. private space for counseling);
- Office space for program staff;
- Trained or qualified staff to run the program and program activities;
- An understanding of the case management process;
- An understanding of evidence-based intervention activities aimed at reducing suicide or self‑harm;
- Access to training in mental health;
- Transportation to mental health services;
- Access to mental health workers; and
- Tele-health access.
The two‑year funding window was also noted to be a significant challenge in the design and implementation of programs.
Despite these barriers, communities do not want to use external service providers or external staff since in the past, this approach has not worked for the community. Communities were said to want to train their own people and use culturally relevant approaches that would resonate with community members and youth.
4.5 NAN Provided Supports
In addition to providing communities with support in application development, NAN provided communities with the following supports:
- Program review: NAN Choose Life staff use an internal program review process to assess whether the programs have been implemented as planned. Specifically, they compare the program description in the application against the program activities described in the annual report;
- Training: NAN has held two training sessions with community Choose Life coordinators. These in-person sessions were held in June and September 2018; and
- Reporting support: NAN staff support communities in completing the annual report.
In the future, NAN intended to increase support available to the communities and provide additional training sessions with the Choose Life Coordinators, as well as establishing a networking group and teleconferences between the Coordinators to allow the sharing of activities and successes. NAN also would like to encourage Choose Life Coordinators to work more in collaboration with community Education Coordinators, although this is not always supported by community leaders who do not always understand the intent of Choose Life programming.
4.6 Gaps in Service
NAN staff noted a gap in mental health services for youth aged 19 to 30, suggesting the definition of youth be extended to allow this group to access Choose Life programming. Funding timelines were said to have made it impossible for NAN to have established a case management approach that could be used across programs as it takes a very long time to establish these relationships. Additionally, communities need more training in proposal development and approaches to suicide prevention.
5. KOSS Choose Life Program
5.1 Background
KOSSS supports approximately 150 students annually from grade 9 to grade 12 who must relocate from their community, without their family, in order to complete their high school education. The communities the youth come from include: Deer Lake, Fort Severn, Keewaywin, McDowell Lake, North Spirit Lake, and Poplar Hill. The students attend urban schools in Thunder Bay, Sioux Lookout, Red Lake, and Pelican Falls First Nation School. Core KOSSS services include administering boarding homes, on-call student transportation and tuition agreements.
Prior to the Choose Life funding, KOSSS had Student Support Workers in place in all four communities, as well as Student Home Workers in the boarding houses. KOSSS was currently piloting a number of same gender student houses that were being funded through INAC (ISC). Parents signed guardianship of the children over to the Student Support Workers while they lived away from home to allow the workers to meet emergent and emergency needs of the children.
5.2 Choose Life Program (KOSSS) Rational
As a result of an increase in anxiety, suicide and self‑harm amongst youth relocated for school, KOSSS implemented the Choose Life program with the following objectives:
- Creating a program that assists students/youth at school while they are relocated;
- Helping students reach success by helping their youth make positive choices; and
- Increase programming by providing supports (e.g. counseling, well-being, mental health, personal growth, opportunities for success, programming, engagement, communication, cultural awareness and healing, personal safety and security, and to empower our students to follow a healthy and successful path; and help students/youth become successful
5.3 Choose Life Program (KOSSS) Program Description
The onset of Choose Life funding allowed the introduction of Well Being Workers in each community, as well as, land based programming, which required the introduction of Land Based Coordinators and Land Based Program Helpers. All students were welcome to participate in the land based activities; although when a student was struggling, they were strongly encouraged to participate.
At the beginning of the school year, the Well Being Workers complete an intake assessment with the students to determine their support requirements with a focus on mental health and well-being. Students also receive an orientation session, plus handbook, that clearly identifies the roles and responsibilities of each of their support workers. The Well Being Workers maintain an ongoing relationship with the students throughout the school year, acting as a support as needed. Well Being Workers may have their office in the school depending upon the community and spend a great deal of time in the school interacting with the students.
The Well Being Workers interviewed all worked closely with the Student Support Workers and other service providers and the school (e.g. mental health workers, psychiatrists, general practitioners managing medications) to coordinate service provision, identify students at risk and generally support the students. Well Being Workers provided information to the Student Support Workers who work with the parents of students, keeping them informed of their child's needs and any services received.
Students participating in the KOSSS program were required to sign contract indicating that they would adhere to a code of conduct. They were allowed three incidents and then they would be sent home. Consequences become more negative with each successive incident. If no incident occurred after the first incident for 30 days, the student's record was returned to zero incidents.
In the summer, the Well Being Workers visit the students in their home community at least once. Well Being Workers noted that summer visits are very important since the visits help to reinforce positive life skills that students have gained while away at school, which may be lost when they return to their home community in an environment that does not foster these skills. Well Being Workers hoped to increase the number of home visits during the next summer break.
Land based programming included activities such as snow shoeing, medicine picking, trapping and hunting. Students were taught technical skills along with life skills during land based activities. Land Based workers strived to involve students in the planning and preparation of all land based activities. Thus, students helped pack equipment and prepare supplies and meals before leaving on an activity. Land Based Workers work closely with schools to keep them informed of upcoming activities and encourage student referral to the program activities.
In addition to land-based programming, Choose Life KOSSS had developed life skill workshops which students could attend.
KOSSS was in the midst of developing an Intervention House, which was slated to open in a week. The Intervention Program would take place at a retreat centre set up by KOSSS. The facility was a converted rural house with shared accommodation for girls (up to four) and boys (up to six), a kitchen, shared living spaces, program room and space for parents to stay. When students were undergoing challenges or had asked to leave the program they could attend the Intervention House for up to five days to refocus and receive the extra support they required to remain in school.
5.4 Choose Life Program Budget (KOSSS)
| Item | Description | Cost |
|---|---|---|
| Salaries |
|
$579,000 |
| $625,000 | ||
| Total Salaries: $1,204,000 |
||
| Benefits | Benefits at 13% |
$156,520 - |
| Rent/Mortgage/Utilities | 12 offices @ $500 per month x 12 months
|
$72,000 |
| $204,000 | ||
| Training | 24 workers at $3,000 per year |
$72,000 $40,000 |
| Travel: Training Well Being Worker Community Visits |
$1,500 per 24 workers to attend training/community 3 x a year: $108,000
|
$108,000 |
| $33,000 | ||
| Land Based Activities | To provide supplies and hire community guides and skilled people, including Elders, for land-based activities: tools for trapping, snowshoe making, boating, snaring, etc.
|
$218,600 - |
| Materials/ Supplies |
|
$245,850 |
|
$114,800 | |
| Computers | 1 New Staff, 3 Staff Sites, 2 desktops each house (Sioux Lookout/Thunder Bay): 10 computers @ $1500/computer and software = $15,000 |
$15,000 |
| Networking | 24 workers @ $500 per month x 12 months | $144,000 |
| Subtotal | $2,541,770 | |
| Administration | 10% of subtotal | $254,177 |
| Total | $2,795,947 |
5.5 Choose Life Program (KOSSS) Challenges
Stakeholders commented that the application process had been difficult and that in the future it would be ideal if the funding agreements for all four KOSSS sites could be combined into a single agreement.
Limited term funding (two years) had made it difficult to hire staff for the positions of Well Being Worker and Land Based Coordinators or Workers, particularly since the positions asked for specific qualifications such as a College or University degree, including the ability to travel using their own vehicle, and provide security checks. Stakeholders suggested that a five year funding period would be more appropriate.
The two‑year funding window also meant that the program had to begin running very quickly leading to insufficient time for program design and to build relationships to support case management. The program was required to develop all of their own templates (e.g. plan or care, release forms, confidentiality forms) and staff suggested that it would have been helpful to have received templates.
The training budget was also said to be insufficient as ongoing staff training was required for new staff hire. Staff turnover was noted to be high due to the demands of the positions. This was strongly noted by Land Based Workers who felt that the position came with many responsibilities that extended beyond those of a 9 to 5 job (e.g. student safety, extended work hours, etc). Well Being Workers suggested it would be helpful if workers could be brought together from all four sites for training and to share best practices. Well Being Workers also expressed the need for more regular debrief meetings; although it was suggested that these were being introduced. Staff generally required more supports to deal with the intensity and stress of the job responsibilities, including training on how to work with students who had undergone trauma. Budgets also need to better account for the number of hours of overtime that staff were required to take on, although they were not able to take sufficient time in lieu as a result of job responsibilities.
A lack of psychiatrists and psychologists made accessing support difficult. Similarly, a lack of support for people in the community was problematic since students experienced more stress during transitions to and from home particularly when their home environment was not stable.
Land Based Workers expressed concerns over the equipment budget noting that many budget line items were to be onetime costs, however, natural wear and tear on equipment meant that it would need to be replaced regularly. Example of such equipment included winter clothing. Additionally, there was no budget for upkeep or maintenance of equipment (e.g. cleaning of winter clothing). Winter clothing for activities was an issue in part because many students came from their home communities without proper winter attire. The Land Based Program Coordinator also suggested that staff required additional training to support land based activities as it was not always possible to find guides with the necessary skills (e.g. first aid, boat license, firearms use). Having the skills in-house could also make the program more cost effective.
Workers also noted that they ended up paying for student snacks on their own since there was no budget item for this and programming took place prior to dinner; sometimes running late.
Lack of clarity and guidance from NAN or ISC on required reporting was said to be a challenge. Program staff had made decisions on what to track but were unclear if they were tracking the correct outputs and outcomes.
5.6 Choose Life Program (KOSSS) Outcomes
Interviewed parents generally felt more comfortable sending their children away to school knowing that there were additional supports available to help the child. Parents reported that their children participated in the land-based activities and showed more confidence as a result. Program support workers also suggested that parents were more comfortable sending their children after the program introduced personal cell phones for each student.
Well Being Workers noted that they had been able to develop a case management approach to working with the students, which included all relevant support workers and the parents. To measure success, KOSSS Well Being Workers tracked the number of incidents by type (e.g. drinking, self‑harming) for the students, as well as, whether they stayed for the full semester and the number of credits they obtained during the semester. It was noted that since the introduction of the Well Being Workers, students were having fewer incidents.
Land Based Workers noted a number of positive outcomes in students who had participated in land‑based activities, including:
- Student acquisition of positive life skills (e.g. the ability to prepare and plan, respect for elders and other people, cooperation, etc);
- Increased understanding of First Nation culture among students;
- Students being challenged and learning that they can meet those challenges;
- Students gaining a better appreciation of their inner strengths and capacity;
- Increased connection with parents and grandparents as students learn traditional practices or land-based skills;
- Increased interaction among students and building of friendships and positive peer relationships; and
- Students taking on leadership roles with friends and new program participants.
Other positive outcomes stakeholders noted among students as a result of the Choose Life program included:
- Increase in the number of students graduating high school;
- Increased retention: typically half of the students went home while in the last year 18 of 23 remained the full year;
- Fewer incidents;
- More well‑adjusted students;
- Less self‑harm;
- Making friends more easily;
- Parents happier with student outcomes (e.g. grades and retention); and
- Youth more talkative and more willing to open up and seek support.
5.7 Choose Life Program (KOSSS) Gaps
A number of gaps were noted in the program, including:
- No student hand off process: by which students could be handed off to post-secondary institutions and new support workers (if available);
- No year round supports and transition supports: to help the students when they returned home for summer or winter breaks as the stressors they left in the community are still there when they return. During transition mental health issues were said to increase. The program was in the process of developing such supports (e.g. tele-health connections, regular summer visits to the community). As an example, safety plans were being developed for when students did not want to return to a potentially unsafe environment or when the student was concerned about the well‑being of a sibling they had left behind;
- A sufficient focus on preventative services: currently program staff were focused on student intake and meeting their current needs. Staff did however acknowledge that the program needed to also include prevention programming (e.g. life skills training, smoking cession programming);
- Need for a student welcome package: Many students were said to arrive with insufficient toiletries and supplies. A welcome package was thought to be needed to help reinforce work later completed by the support workers to teach the students about self‑care and hygiene.
- Need to improve parental involvement: It was noted that there was still a need to better engage parents in their child's education/care while away from home. Additionally, stakeholders suggested that the whole family commonly requires help and that addressing the needs of the student without addressing precipitating factors in place in the home will not result in a sustainable solution for the child;
- Insufficient spaces to meet student demand: More students request to participate in the land based activities than the program can accommodate;
- Student in-take timelines: Well Being Workers indicated that the number of students to Well Being Worker means that some wait a long time for intake assessment, which can result in negative consequences for the child;
- Lack of standardized validated intake assessment tools: It was noted that Choose Life sites did not use standardized in-take assessment tools that could identify mental health issues in the students when they arrived. In order to implement such an approach the appropriate tools would need to be identified and all Well Being Workers would need to be trained on how to use the tools. This would ensure that all workers could proactively identify issues among students and refer them for diagnosis and treatment as required. It would also allow all staff to speak the same language with respect to mental health; and
- Poor or undetermined linkages between program activities and positive mental health outcomes: It was stressed that current programming was not proven to act as a protective factor in mental health and that programming should focus more on prevention and promotion of mental wellness with greater reliance on standardized mental health assessment tools and trained mental health professionals.
6. Lac Seul Choose Life Program
Lac Seul First Nation is comprised of three distinct settlements: a) Frenchman's Head; b) Kejick Bay; and c) Whitefish Bay. As of October 2015, the on-reserve population was about 860 with a total registered population of 3,372.
The Lac Seul Choose Life program had only begun operating at the end of April 2018. Since then, the program had been able to:
- Develop job description (roles and responsibilities) for program staff;
- Begin filling job openings;
- Worked with the Mashagama community to learn about their Choose Life program;
- Begin collaborating with community stakeholders (education, social services) to allow their staff to refer to the Choose Life program;
- Completed community open-houses to gather feedback on the types of programming community members would like to see developed;
- Purchase equipment;
- Develop program templates and forms (e.g. registration forms);
- Developed a program tracking database;
- Begun training staff (e.g. staff attended a land based program conference, visited other communities to observe their program); and
- Run a few land based programs (e.g. medicine picking with a traditional healer, and two hunting and fishing trips).
Program demand for all activities was greater than the programs capacity. In the future, the community plans to develop a wellness camp, which would be used by the Choose Life program.
The program is still working on developing a program manual and program description that could be used to educate community members about their services.
Staff and stakeholders noted that the process of program development and implementation had been challenging and that the program would have benefitted from greater support from NAN or the funder in:
- Program design;
- Land based programming;
- Strategic planning;
- Mental health intake assessment processes and tools;
- Understanding how to integrate parents into programming;
- Best practices; and
- Measurement and assessment of outcomes.
7. Lessons Learned
When considering how to implement similar programming in other First Nation on-reserve communities across Canada, Choose Life provides lessons relevant to mental health programming. However, as noted earlier the review of Choose Life was very preliminary and did not capture the full depth and range of services. Lessons can be taken from the administrative and community program delivery level:
Need for program design supports: The Choose Life program as overseen by NAN struggled with the short funding timelines. NAN did not have existing staff and processes in place to support communities prior to the onset of funding so they were required to develop capacity while delivering programming. This meant that NAN was unable to provide many supports to communities beyond assistance with application completion. Ideally, a program of this nature would be given sufficient time for the administrative organization (NAN) to hire and train internal administrative staff, develop processes and auxiliarysupports that could be accessed by the individual community programs. Internal administrative staff thus required training on application completion (what makes a good application), program design (what makes a good program), outcome measurement (how do you think program activities translate to outcomes), and program monitoring (what outputs and outcomes should be measured to demonstrate success). Examples of supports that then could have been developed by the administrative organization and made available at the community level would include:
- Workshops outlining Jordan's Principle;
- Workshops on application completion;
- Workshops and toolkits on program design;
- Workshops and toolkits on theories of change, logic models and program monitoring and measurement;
- Toolkits with commonly used program protocols such as intake forms and consent forms; and
- Workshops on Human Resources processes for hiring, contract development, etc.
Need for clear program theory underpinning programming activities: As noted previously, programs were unclear if the activities they were completing clearly linked to positive mental health outcomes. Good program design requires sound theories of change that show the link between program activities and the desired program outcomes. Just developing such a robust program theory and implementing it could take a two-year period. At the community level, communities did not have the capacity to complete such a task, and as noted above, nor did the administrative organization. Time is required for the administrative organization to build this capacity prior to rolling out program funding. Thus program design funding is required prior to program funding.
Communities understand the needs of their members: The programs visited had a solid understand of the challenges and needs in their community. Further, they had creative and innovative ways to address those needs; however, they did not clearly understand how these innovative ideas could link to positive mental health outcomes. This is not to suggest that a top down approach to program design is required, instead, programs need support in making linkages between their program activities and the desired outcomes.
Clear direction on program monitoring is required: It was noted that at the community-level and NAN-level, programs were unclear on what should be monitored and reported back. Thus, the Jordan's Principal funding envelop would ideally provide clear direction on what program data should be collected and reported back to the funder.
Support with mental health assessment and promotion/prevention is required for good mental health programming: The capacity to support mental health is lacking in most communities across Canada. Mental health workers are sparse, stigma around mental health is high, and understanding of the necessary protective factors is limited among the general population. When providing funding for a targeted program area of this nature, funding should come with training in mental health. Thus for Choose Life, stakeholders suggested that mental health resources should have been made available to all community programs, including:
- Appropriate assessment and intake tools (and where to obtain training to implement them);
- Appropriate triage process when mental health issues are identified; and
- Evidenced based mental health prevention and promotion activities.
Appendix C: Early Childhood Intervention Program Regina Case Report
SASKATCHEWAN EARLY CHILDHOOD INTERVENTION PROGRAM
Program Review – Community Visit Summary
(Regina, Children North (La Ronge) and Northeast ECIPs)
September 24-26, 2018
1. Background
The Early Childhood Intervention Program (ECIP) Regina provides services to 18 Saskatchewan First Nations.Footnote 26 These include: Carry the Kettle, Cowessess, Day Star, Fishing Lake, Gordon, Kahkewistahaw, Kawacatoose, Little Black Bear, Muscowpetung, Muskowekwan, Ochapawace, Okanese, Pasqua, Peepeekisis, Piapot, Sakimay, Standing Buffalo and Star Blanket.Footnote 27
2. Method
For the case study of the ECIP project in Saskatchewan, discussions were held with ECIP executive directors from three regions (Regina, Children North (La Ronge) and Northeast ECIP). However, the detailed case study was limited to the Regina ECIP. The Jordan's Principle program that was examined was the additional funding provided to Saskatchewan ECIPs in fiscal year 2016‑17 to allow ECIPs to provide services to First Nations youth aged 6 to 17 with complex health conditions.
As part of the review, the researchers conducted the following interviews:
- Group interview with three executive directors who were responsible for ECIP programs in Regina, Children North (La Ronge) and the Northeast regions;
- Interviews with ECIP staff, including two Specialized Support Function staff, as well as ECIP program director and ECIP Executive Director (Regina ECIP);
- Interviews with other partners and service providers (n=6), including school board officials (Superintendent of Schools, Director of Special Education), Special Education teachers, Manager from the Ministry of Social Services, contracted service provider, member of ECIP Board of Governors (Regina); and
- One on one interviews with 13 parents plus one parent focus group with six parents.
3. ECIP program overview
3.1 Program History
This program came to fruition in Saskatchewan in 1980 (Health Canada, 2017: 1). At this time, children aged 0-6 who were experiencing a variety of developmental delays such as "genetic, environmental, medical or organic conditions that require interventions for language, gross and fine motor, visual, hearing and behavioural challenges" were eligible for community based supports (Health Canada, 2017: 2). Initially, the program was funded by the Saskatchewan Ministry of Education (provincially), and by FNIHB. It is now funded through Jordan's Principle (Health Canada, 2017: 2). INAC (now two departments referred to as Indigenous Services Canada and Crown-Indigenous Relations and Northern Affairs Canada)Footnote 28 originally funded the program for First Nation Communities in Saskatchewan before FNIHB-Saskatchewan took over in 2014 (Health Canada, 2017: 2).
In fiscal year 2016‑17, ECIPs in Saskatchewan applied for additional funding under Jordan's Principle to extend services and supports to First Nations youth aged 6 to 17 years of age (or up to 21 years if still in school) including youth who lived on-reserve. Under this "new" program, the ECIPs across the province undertook a variety of activities. A common program element of these programs was however, the hiring of "specialized support facilitators" (SSFs) whose role was to coordinate the provision of services to parents and children. In addition, each region could also utilize Jordan's Principle funding for other activities. For example, whereas Regina ECIP hired two specialized support facilitators, other regions tended to hire only one such facilitator but implemented other programs or services. For example, in the Children North (La Ronge) ECIP, in addition to the hiring of one SSF, the ECIP also established a mentorship program where First Nations Elders/Role models would work with at risk First Nations youth in terms of assisting those who may have mental health/other health issues. In other regions, in addition to the SSF, some regions hired specialized clinicians (i.e. Speech Language Pathologists, Occupational Therapists etc.) to provide home based services to First Nations youth (this was done due to the challenges of getting such professionals to visit rural remote communities to provide such services).
A major role of the SSF workers were to serve as an advocate for First Nations parents and children. This typically meant undertaking liaison with the school to ensure that students were receiving appropriate services in provincial schools, as well as to coordinate with local health authorities as appropriate. In addition, the SSF/ECIPs also served to manage parent applications to Jordan's Principle to obtain such supports as respite, assistive technologies, or other services (Equine Assisted Learning) as required.
It should be noted that funding for the additional programming offered by the ECIPs in Saskatchewan ends on March 31, 2019.
3.2 Program Objectives
ECIPs have existed in Saskatchewan for more than 20 years and were established to provide support to those children who either at risk for, have a diagnosis of, or exhibit developmental delay. The program is available to all children aged zero to six throughout Saskatchewan and includes both First Nations and non-First Nations youth.
The overarching goals of ECIP include:
- Maintaining or enhancing the development of children in the ECIP program;
- Increasing the knowledge of families in reference to their child(ren)'s and family needs and strengths;
- To develop and increase the families' advocating abilities for those who either experience or are at risk for developmental delays; and
- To create more inclusivity within the community "as families connect to other programs and services that meet their needs".
For the purposes of the additional Jordan's Principle funding received in 2016‑17, the objectives of the ECIP were further expanded to include the provision of specialized support to First Nations families and youth aged 6 to 17 (and up to 21 if still in-school) with complex health needs.
4. ECIP Jordan's Principle Program Operations
Each ECIP in Saskatchewan (14 ECIPs) are overseen by a local Governance Board for each ECIP appointed by the province. ECIPs are non-profit entities primarily funded by the Saskatchewan Ministry of Education although ECIPs will also receive funding from a variety of other organizations. In terms of the provision of services to First Nations youth, while ECIPs have traditionally provided services to both on- and off-reserve First Nations youth aged 0 to 6 years of age, in 2016-17, the ECIPs received additional funding under Jordan's Principle to extend services to cover First Nations youth aged 0-17 (or up to 21 years if still in school). As noted previously, this funding has been typically used to hire specialized support facilitators, as well as fund other services such as mentorship programs or the hiring of clinicians to provide direct services.
It should be noted that there is no overarching coordinating body for the 14 ECIPs across Saskatchewan. This means that the ECIPs themselves will organize themselves and develop common positions with respect to programs and policies. It also means that it is somewhat difficult to establish "common" provincial approaches to service delivery, standards or training as these second level support functions do not exist.
4.1 Staff
In general, the ECIPs utilize existing administrative support functions to manage the program. Under the Jordan's Principle funding received in fiscal year 2016‑17, the ECIPs were provided with limited administrative funding to manage the additional services to be provided, including the hiring and management of SSFs, management of other programs and services (mentorship, Speech Language Pathologist, OTs), as well as cash management of parental applications made directly to access funds under Jordan's Principle.
For the purposes of the review, analysis of the impact of Jordan's Principle funding was focused on the additional programs and services provided in the fiscal year 2016‑17 funding allocation. As noted previously, each ECIP could identify what services were needed in the community and design programs appropriate to their specific communities. While almost all ECIPs established a specialized support facilitator position (typically a contract position), the other services introduced varied on the requirements of the region. In Regina, given the relative close proximity to special clinicians, it was decided that they would hire two SSFs to provide services. In contrast, rural and northern ECIPs reported that they had difficulty in obtaining specialized clinician services (Speech Language Pathologists, OTs), so, in some regions, they developed special contracts with such professionals to provide services on a "staff" basis (and only hired one SSF). Other regions introduced other programs such as mentorship and even land-based programs as appropriate.
In most regions, the Executive Director of the ECIP will manage the additional programs and services funded under Jordan's Principle since 2016‑17. The directors interviewed as part of this research indicated that they spent much time early on in the program to design the program (including conducting consultations with First Nations communities as to what the program should do), however, now that the program is in operation, they spend between 10 percent to 15 percent of their time managing this additional programming provided under Jordan's Principle funding. The ECIPs also use existing administrative staff to handle the "cash management" of parent applications to Jordan's Principle (i.e. will pay service providers directly so that parents are not out of pocket waiting for funds to arrive from Jordan's Principle).
4.2 Services
In examining the additional services provided by the ECIPs under the 2016‑17 Jordan's Principle funding, there emerges several core activities/services provided across almost all ECIPs in Saskatchewan. These include:
- Establishment of a "coordinator" position (SSF) whose role was to serve as an advocate for the child and to coordinate service needs of First Nations youth aged 6-17 (or to 21 for special cases) that included the parents, schools, and other health/social service agencies.
- As appropriate, implement specific programs/services that addressed unique regional needs. This could include for example, establishment of a mentorship program, development of land-based cultural programs, and/or the hiring of clinical specialists (Speech Language Pathologists, Occupational Therapists etc.) to provide direct service to youth.
- Via the SSF's assist in the submission of applications to Jordan's Principle by parents to access additional supports including respite, assistive technologies, and other services as necessary. Typically, many ECIPs also managed the cash management of such services where they would pay for the services and obtain reimbursement from Health Canada so that parents were not "out of pocket" for such expenses.
4.3 Partnerships and Service Providers (Regina ECIP)
Just prior to the launch of the 2016‑17 program, ECIP staff conducted consultations with First Nations communities as well as local service agencies. The goal of such consultations were to better understand the needs of the communities (with respect to the health needs of First Nations youth aged 6-17) as well as to provide information as to the services that could now be provided via the additional Jordan's Principle funding.
The program has established a number of partnerships or working relationships, which allow the provision of services to children with complex needs within the community. In Regina, this included relationships with both the public and Catholic school boards as well as the local regional health authority. In addition, relationships were also expanded to include the Saskatchewan Department of Social Services and other social welfare agencies as appropriate.
It should be noted that due to the very tight timelines for the roll-out and implementation of the program, ECIP stakeholders noted that they had to often "develop policies and procedures on the fly" and as such, they did not have extensive documentation as to what the program could/could not do that could be shared with other service partners. In discussions with Service Partners, it was noted that it was often the SSF who communicated key program elements to other service providers. For example, in discussion with local school officials, they noted that until the SSF arrived, they were unsure as to what additional services/support would be provided to First Nations youth, aged 6 to 17 years, with complex medical conditions as part of the additional funding provided in fiscal year 2016‑17.
4.4 Program Outreach
As noted previously, the ECIP staff conducted a series of consultations with the respective First Nations communities as well as other education and health and social service agencies. These consultations occurred prior to program roll-out to explain key program elements as well as the role of ECIPs in now supporting older First Nations youth with complex health conditions. In the Regina ECIP, the SSF coordinators are key to establishing relationships with likely referral agencies, including health/education coordinators in the First Nations communities, local school boards, the regional health authority and the Ministry of Social Services to name a few.
It was noted that ECIPs were promoting the program directly to parents and/or caregivers via the ECIP website (although there appears to be only limited information on the Regina ECIP website about the program). In addition, in discussions with the SSFs, it was noted that parents were becoming more aware of the program through "word of mouth" and other unofficial communication/promotion.
4.5 Scope of Service Provision
Information provided by the Regina ECIP suggests that the region is currently directly supporting approximately 70 parents in which the SSFs are providing direct support. In addition, the ECIP may also assist First Nations parents in terms of accessing Jordan's Principle funding for additional supports such as respite, purchase of assistive technologies and/or other supports.
It should be noted that in the Regina ECIP, the key program element is the establishment of the SSF function, which is designed to be an advocate/case management service for First Nations parents and children with complex health conditions. In this context, the Regina SSFs serve as a "program navigator" for First Nations children/families in terms of helping ensure that such families are supported in their application to Jordan's Principle funding for additional supports, or to coordinate services provided by schools/local health authorities/and other health providers as required.
Other ECIP executive directors interviewed as part of this review noted that the additional Jordan's Principle funding allowed for the hiring of a SSF, and that the funding also allowed for other services, including:
- Learning and behavioural assessments;
- Physiotherapy and occupational therapy;
- Speech and language therapy and audiology therapy;
- Visual therapy;
- Behavioural/cognitive behavioural therapy;
- Psychologist and psychiatrist consultations, spiritual wellness supports, and mental health therapy;
- Child development supports (individual);
- Mentorship programs; and
- Land-based cultural programs.
A key element of the services provided by all ECIPs was to support parents in completing applications to obtain funding or support from other health and social service agencies as well as Health Canada (Jordan's Principle) to provide additional supports to the child and/or families.
SSFs and parents most commonly reported that the SSFs were key in helping parents with applications for assessments, assistive technologies (i.e. obtaining an IPad for use at home with the same software as IPads provided to youth in the schools), respite as well as other learning/behavioural therapies (i.e equine assisted learning). It was also noted that the SSFs played a major role in terms of advocating for the parents/children to get other supports/services from other agencies. For example, several parents noted that the SSF was instrumental in terms of getting the local health authority/other agency to fund needed home adaptations.
It was strongly felt that the SSF played a key role in terms of providing needed support to parents with children with complex health needs. As noted by a First Nations parent interviewed, the SSF role has played a major role in terms of reducing the isolation and frustration of First Nations parents in terms of accessing needed supports.
"the SSF coordinator is great..they are actively helping me access the supports I need for my daughter..in the past, I felt that I had to fight the system to get help for her, now, with the SSF coordinator, I feel that I have someone in my corner fighting for me and my daughter..it is a real Godsend"
4.6 Program Budget
The executive directors interviewed as part of the case studies noted that they provided financial information to Health Canada in their regular annual reports and could not release this information without Board approval. (Note: the consultants have recommended that ISC obtain these annual reports from Health Canada as part of this review.)
To date in the Regina ECIP, it appears that the funding is sufficient to allow for the two SSFs to manage an appropriate caseload (approximately 30-35 families per worker). It was noted that there was no wait list for parents to access the SSF, although it was unclear as to whether there may be other waitlists (i.e. waitlist for assessments, waitlist to see psychiatrist, other clinicians).
While the Regina ECIP receives funding for program administration, the Jordan's Principle funding is maximized in that the ECIP did not have to hire additional staff to manage or provide administrative support for the Jordan's Principle funded activities. It should be noted, however, that the Regina ECIP Executive Director felt that the 10 percent allocated to program administration was insufficient due to the amount of work being done by the ECIP to manage family applications to Jordan's Principle and the cash management of approved requests (i.e. confirm provision of services, pay for service providers directly etc.).
4.7 Monitoring of Child and Family Outcomes
In general, the Regina ECIP does not have an established program monitoring framework for the additional Jordan's Principle funding received. The program monitors the number of children case managed by each FFS, and tracks the number of Jordan's Principle applications submitted and managed by the ECIP. It was noted that in the future, Health Canada should identify what program outcomes/impacts should be monitored and reported (and, as appropriate, provide sufficient funding to support such reporting). In discussion with ECIP coordinators, it was noted that there could be several measures that could be implemented to assess program impacts. Among these include:
- Use of standardized assessment tools such as the Assessment, Evaluation, Programming Systems, which could measure development of the child over time;
- Wait lists;
- Use of time based monitoring including length of time to receive assessment, and length of time prior to receiving service from specialized clinicians (Speech Language Pathologist, OT, other);
- Family survey (ECIPs used to do this but have since discontinued their family survey due to funding pressures); and
- Service provider/partner survey to assess program impact.
It was also noted that the program could demonstrate net impact using a Social Return on Investment approach in which the positive outcomes observed could be contrasted against the increased costs that would be incurred if there was no improvement in youth health or education level. For example, service partners noted that with the increased use of respite services, there were fewer parents who were committing their children to the province for temporary guardianship (which was very costly to the province). Similarly, the representative from the Ministry of Social Services noted that with the supports provided to at risk youth with behavioural issues, they had more opportunities to "close" client files given that such youth could be discharged and receive required services to support such youth in their transition back into the community. Furthermore, the stakeholder noted that with the introduction of Jordan's Principle funding for youth aged 6 to 17 years of age, they were seeing fewer youth "returning" to the Ministry than had been the case in prior years (i.e drop in youth recidivism).
4.8 Program Outcomes
Despite the lack of formal performance measurement frameworks or outcomes reporting, the site visits did collect anecdotal information as to early impacts of the program. Of course, this data was qualitative in nature and cannot be construed to be representative of all outcomes experienced by children and/or parents. These various program outcomes as reported by parents and stakeholders include the following:
Improved Educational Outcomes. Teachers interviewed as part of this research noted that the children who were now being supported via the Jordan's Principle funding were benefitting from such supports. Educators cited such improvements as increased school attendance, improved academic scores (due to tutoring and other supports) and access to additional educational supports given that some student assessments were "fast tracked" due to the ability of using Jordan's Principle funding to obtain such assessments.
Enhanced Parent Well-Being. Parents gave high praise for the work done by the SSFs to help secure funding for respite services. Parents noted that in the absence of such support, they often had no recourse but to temporarily "sign over" guardianship of their children to Child and Family Services as they could not cope with the 24/7 demands of their children. In addition to providing relief for parents, many parents structured their respite services to provide additional supports to their children. For example, some parents mentioned that they used respite dollars to purchase tutors, or to hire "behavioural interventionists" to help with the socialization of their child. Almost all parents talked about being better "able to parent" because of the supports provided by the SSF as well as the Jordan's Principle funding for required supports/services. Parents were also very positive in the way the Jordan's Principle program operated in Regina. That in general the FFS would identify what services/supports that they should apply for, assist such parents in applications, and generally serve as an advocate in their interactions with other education, health and social service agencies.
Improved Service Coordination/Case Management. Educators noted that the SSF now provided a better link between school supports and broader community supports. As noted previously, the stakeholder from Child and Family Services noted that "at risk" youth with anger/behavioural issues would previously be discharged from the Ministry, but, without any community supports, would often end up back in Ministry care. By using the services of the FFS (as well as other Jordan's Principle funded supports), it was felt that the risk of recidivism for such youth was reduced. In addition, it was felt that the FFS would help coordinate the services received from the school as well as community health and/or private services.
4.9 Program Challenges
Notwithstanding the high level of support for the work done ECIPs in terms of supporting parents with children with complex health needs, stakeholders and parents identified several issues that affected service delivery and planning. These challenges are:
- Possible service overlap. ECIP executive directors noted that the program was rolled out very quickly and without sufficient advance planning and service coordination. For example, in one ECIP, they decided to hire a Speech Language Pathologist to provide direct service to identified children. The ECIP was surprised to learn that while they were delivering this service, Health Canada funded a nearby First Nations Band under Jordan's Principle to hire a SLP to work with many of the same children who were receiving service from the ECIP SLP. The ECIP stakeholders noted that the first stage of funding should go to the establishment of a "Community Service Map" that identifies what services are available, what services are missing, and what agency would be responsible for addressing such service gaps.
- Limited Funding Window. The ECIP coordinators noted that they had a very short time to get the program up and running, and now that they have the program staffed, there will be issues in terms of staff retention as funding is scheduled to end as of March 31, 2019. It was felt that the program needed a longer funding window (three to five years) to allow for the reasonable roll-out and administration of the program.
- Limited Understanding of the Role of Jordan's Principle funding. Parents and some stakeholders noted that it was not clear whether Jordan's Principle funding was to the first, second or last funding source. Parents noted that often they were told that they needed to apply to other agencies for supports (i.e. home adaptation) and only apply for Jordan's Principle funding if they were denied by the other organization. The ECIP coordinators noted that better information as to what Jordan's Principle would/would not fund would help streamline the application route used by parents.
5. Lessons Learned
Review of the ECIP program as applied to youth aged 6 to 17 with complex health conditions was undertaken with the objective of identifying how such a program could be implemented in other jurisdictions.
The review (document review, site visit and key informant interviews) highlighted several key factors, which contributed to the program's past and continued success. These factors are discussed below.
Presence of Regional Early Childhood Network: The success of the Jordan's Principle funding used to support children and parents with complex health conditions in Saskatchewan is in part a testament to the existing infrastructure in place in the province. The system of ECIPs in Saskatchewan is not common across Canada. With a focus on children with developmental disabilities, the ECIP network is well integrated with schools, other social service agencies and clinicians (SLPs, OTs, other). In this context, provisions of additional funding to provide supports to First Nations youth aged 6 to 17 with complex health needs did not require a major investment in a new service delivery structure (was a "add on" to the service model already in use in Saskatchewan).
Enhanced Community Planning and Service Coordination: It was noted that the ECIPs undertook consultations with First Nations communities as to what programs/services should be provided in each region to best meet child/community needs. However, it was noted that ECIPs were only one of several agencies that received funding under Jordan's Principle to provide series to at risk children. In the future, it was noted that more planning should be undertaken, with the goal of creating a "community service map" that identified service gaps and could assign program responsibility to specific organizations. Again, a common issue raised by the ECIPs was the very limited time available to do a proper program roll-out that would have included better/enhanced coordination with First Nations communities and/or other service providers.
"Wrap Around" Model of Case Management: It was felt that the SSFs played a critical role in terms of assisting First Nations parents access appropriate services and supports for their children. SSFs themselves described their case management approach as a "wrap around" model that included the child, the parents, educators and other community supports. This model helped ensure that there was a consistent service plan developed for the child and that all service providers had a good understanding of the role of each other in terms of assisting the child. Parents almost universally noted that access to the SSF greatly increased their confidence that their children would receive appropriate service.
Infrastructure: As noted previously, the success of the Jordan's Principle funding in Saskatchewan can be attributed to the presence of an existing child and youth service network in the province. The ECIP infrastructure meant that most Jordan's Principle dollars could be used to directly support service delivery, as no additional structures would be needed to support overall program administration. In this context, extension of the program funded in Saskatchewan, to other jurisdictions, may require a much different funding model if such structures do not exist in other regions.
Program Monitoring: It was noted that reporting requirements specified by Health Canada focused on financial details (how funds were spent) but had little in terms of the impact of such expenditures. Although ECIPs report on the number of children served, it was noted that it would be important to collect data that documents the impact of Jordan's Principle funding. This could include, for example, changes in assessments, increased education outcomes, or even family satisfaction. ECIPs noted that such a different reporting approach would provide more crucial information as to the success of the program as opposed to the current activity based reporting. Stakeholders noted that a portion of future funding should be allocated to the establishment of appropriate systems to monitor and track outcomes rather than the current financial and activities focus of the current reporting structure.